|
|
|
| |
| |
| |
| |
Medical Pharmacology Lectures: Cardiovascular Pharmacology, Antihypertensive Agents Slide 2
press ![]() above to
begin the lecture
above to
begin the lecture
and install current free versions of Quicktime, if needed, to support lecture series audio!
|
|
Considerations: Anesthetic Management in Hypertensive Patients
Hypertension: Organ Systems Effects
Normal control of BP: sympathoadrenal axis-- response to a decrease in BP
Sensed by Central baroreceptors {heart & great arteries}
Stimulation of ß-adrenergic systems
increased heart rate (positive chronotropic response)
increased force of contraction (contractility, positive inotropic response)
increased renin secretion {juxtaglomerular renal cells}
Stimulation of alpha-adrenoceptor systems: causes vasoconstriction
With essential hypertension, above mechanisms function inappropriately
Excessive sympathetic activation
Elevated norepinephrine may promote through vascular endothelium injury:
vascular hypertrophy
atherogenesis
ß-adrenergic receptor down-regulation
Reduced endothelium-mediated vascular relaxation
Consequence: increased vasoconstrictive tone (chronic vasoconstriction)
Excessive sympathetic activation promotes enhanced peripheral vascular resistance in hypertensive patients
Hypertension and the kidney:
ß-adrenergic receptor stimulation leads to increased renin secretion which in turn leads to increased angiotensin II levels
Increased angiotensin II levels promotes an increase in BP by means of:
direct vasoconstriction
increasing renal cortical {zona glomerulosa}aldosterone production which causes intravascular volume expansion
Hypertension associated with elevated renin levels may predispose patients to myocardial infarction {compared to those patients with normal/decreased renin levels}
Hypertension associated with elevated renin levels is amenable to treatment with ACE inhibitors {e.g., captopril (Capoten)}
"Pressure-naturesis"-dysfunctional in hypertensive kidneys {Definition of pressure-naturesis: increasing Na+ & H2O excretion by the kidney with increased blood-pressure}
Frequency: 4%-5% of hypertensive patients
Principal causes:
Endocrine
Renal
|
Cushing's syndrome |
Hyperaldosteronism |
Pheochromocytoma |
|
|
|
Pheochromocytoma
|
Hulyalkar, A. R., and Miller, E.D., Evaluation of the Hypertensive Patient in Principles and Practice of Anesthesiology (Longnecker, D.E., Tinker, J.H. Morgan, Jr., G. E., eds) Mosby, St. Louis, Mo., pp. 157-165, 1998.
Goldfien, A.,Adrenocorticosteroids and Adrenocortical Antagonists, in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp 635-650.
Williams, G. H and Dluhy, R. G. , Diseases of the Adrenal Cortex, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, pp 2035-2056.
![]()
Early Cardiac problems associated with chronic hypertension
Diastolic relaxation abnormalities (may be subclinical)
Such diastolic dysfunction may manifest during surgical stress
Identification of diastolic dysfunction: echocardiography (Pulsed-wave Doppler)
Abnormal filling characteristic secondary to diminish left ventricular compliance (increasing ventricular wall stiffness)
Angina:
May occur in the absence of coronary vascular disease-- secondary to reduced coronary flow reserve
Transient myocardial ischemia may occur in the absence of coronary vascular disease in these patients {frequency = 50%}
Probable mechanism: abnormal coronary flow reserve {ischemia unrelated to left ventricular hypertrophy}
Left ventricular hypertrophy:
Reversibility: dependent on antihypertensive protocol
ACE inhibitors (e.g. captopril (Capoten)) or the calcium channel blocker verapamil (Isoptin, Calan): effective in reducing left ventricular hypertrophy
Other agents useful in left ventricular hypertrophy management:
Methyldopa (Aldomet)
Calcium channel blockers
|
|
Risks associated with hypertensive cardiomyopathy and caused by myocardial ischemia {secondary to increased myocardial oxygen demand & reduced coronary flow reserve
Sudden Death
Ventricular Tachyarrhythmias
Abnormal ventricular compliance: major characteristic of hypertensive cardiomyopathy
Systolic function significantly limited in end-stage disease
Sequence in chronic hypertension:
Slow increase in left ventricular diastolic pressure (preload) leads to reactive fibrosis + hypertrophy [Increased hypertrophy reduces wall tension] which causes monocyte necrosis & reparative fibrosis {ACE inhibitors, e.g. lisinopril (Prinvivil, Zestril) may prevent reactive fibrosis but reparative fibrosis may be irreversible}
Ventricular hypertrophy -- significant wall thickening -- predisposes to ventricular arrhythmias
Hypertrophic & fibrotic myocardium associated with patients who have both diabetes & hypertension
Captopril (Capoten)
Adverse Effects
|
* Laplace equation, T =PR/h, where T = myocardial wall tension; P = left ventricular end diastolic pressure; R = radius; h = wall thickness -- recall that as wall tension increases, myocardial oxygen requirement increases, predisposing to anginal episodes
Hulyalkar, A. R., and Miller, E.D., Evaluation of the Hypertensive Patient in Principles and Practice of Anesthesiology (Longnecker, D.E., Tinker, J.H. Morgan, Jr., G. E., eds) Mosby, St. Louis, Mo., pp. 157-165, 1998.
Stoelting, R.K., "Calcium Channel Blockers", in Pharmacology and Physiology in Anesthetic Practice, Lippincott-Raven Publishers, 1999, p. 352-353.
Hypertension & Stroke
Reduction in BP reduces stroke incidence
Hypertension predisposes to both ischemic & hemorrhagic stroke
Mechanism:
Hypertension damages vascular endothelium and in turn damaged endothelial cells promote:
(1) localized platelets aggregation
(2) thrombus formation and
(3) atheromatous plaque formation
Plaque formation reduces distal flow
Reduced vessel lumen dimension promotes turbulent blood flow which causes further injury
Smooth muscle media hypertrophy may weaken vascular integrity, increasing the likelihood of hemorrhagic stroke
Thrombotic Stroke
Acute thrombus at site of vessel narrowing
If a portion of the thrombus breaks off, distal vessel plugging results in embolic stroke
Predisposing factors for embolic stroke:
Cardiac arrhythmias
Atrial fibrillation (myocardial thrombus formation leading to cerebral emboli)
Hypertension predisposes the myocardium to arrhythmias
Infarcts secondary to hypotension, when BP falls below range of cerebral autoregulation
{Watershed infarcts = insufficient systemic blood-pressure for arterial blood to reach the end of vascular branches-- in particular poor cerebral cortical perfusion of a susceptible "watershed zone" between anterior & middle cerebral artery or middle & posterior cerebral artery may result in linear infarcts}
In the chronically hypertensive patients, a greater blood-pressure is required to maintain adequate cerebral perfusion compared to normal patients

Watershed Infarct image courtesy of the Digital Slice of Life Cooperative Project
Chronic Hypertension: Renal Effects
Chronic renal injury
Intimal hyperplasia
Afferent arteriolar sclerosis
Parenchymal fibrosis
secondary to reduced blood flow
Reduced renal function as a result of hypertension is characterized by a gradual degradation in renal function {benign nephrosclerosis}, leading to ultimately a rapid and irreversible renal failure {malignant nephrosclerosis}
Characteristics of benign nephrosclerosis
Renal dysfunction probably due to compensatory hyperfiltration by normal glomeruli
Increase glomerular pressure is associated with proteinuria
Hyperfiltration of certain glomeruli tends to induce sclerosis of otherwise normal glomeruli
Malignant Nephrosclerosis
Renal manifestation of malignant hypertension
If untreated (initially with IV vasodilators), malignant hypertension will precipitate renal failure within days-weeks
Treatment: typically IV vasodilators initially {e.g., nitroprusside sodium (Nipride), nitroglycerin}
Three renal histological changes associated with malignant hypertension
Arteriolar fibrinoid necrosis
Hyperplastic arteriosclerosis {arteriolar "onion-skinning"-note the vessel in the center of the image below}
Glomerulitis in the hypercellular glomerulus {screen position: 7 o'clock position below}
Description and image: courtesy of The Urbana Atlas of Pathology, use with permission
Malignant Nephrosclerosis Images
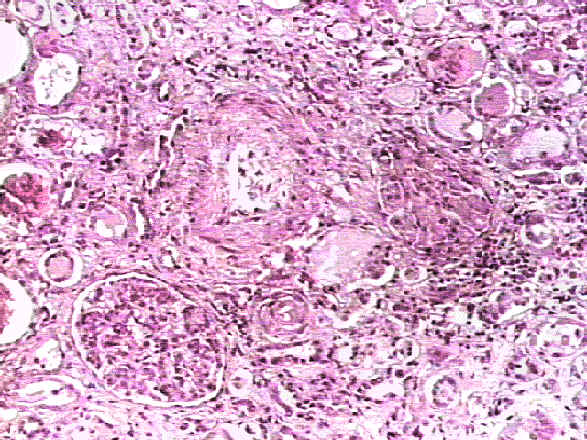

Image contribution by Saint Francis Hospital
Hulyalkar, A. R., and Miller, E.D., Evaluation of the Hypertensive Patient in Principles and Practice of Anesthesiology (Longnecker, D.E., Tinker, J.H. Morgan, Jr., G. E., eds) Mosby, St. Louis, Mo., pp. 157-165, 1998.