|
Overview
-
3Patient
Assessment-Estimating the extent and basis of patient anxiety
-
Psychological factors to consider
-
Appropriate levels of fear-the
anesthesia provider may help set the patient's expectations:
-
Presurgical explanations should
take into account the anxiety-state of the patient, i.e. a
very anxious patient may have even further anxiety as a result
of such discussions
-
Anesthesia providers may aid
the patient in coping with preoperative anxiety by suggesting
that patients focus their attention to other more pleasing or
at least distracting activities
-
Examples of effect of coping
mechanisms which can be promoted by the anesthesia provider
-
Helping the patient view
themselves as part of rather than separate from the
health-care providing team. This type of
"empowerment" reduces the likelihood of the
patient regarding himself as an "victim" and can
help the patient recognize their role in the
decision-making process that led to surgery
-
The anesthesia provider may
help the patient assume a level of control concerning
their environment and situation-for example use of
breathing control in promoting relaxation. Providing
opportunities for control may be especially important for
children and young adolescence -- for example allowing a
child to choose on which finger the pulse oximeter is to
be placed would be such an example
-
Relaxation methods: The
anesthesia provider may suggest contraction/relaxation
cycles of muscles in a small region, such toes or
ankles
-
Mental
distraction-such music, selective attention,
etc. approaches which promote relaxation may be
useful.
-
Time of administration: 1-2 hours
before anesthesia induction
-
Outpatient setting: IV
premedication just before surgery
-
Primary goals for premedication (premedication
agents may include antihistamines, antiemetics, alpha2
adrenergic receptor agonists, antacids, histamine receptor (H2)
antagonists, opioids, benzodiazepines, gastrointestinal
stimulants)
-
Anxiolytic effects -- reduction
in patient anxiety with expected reduction in
circulating catecholamines
-
Sedation
-
Reduction in preoperative pain
(analgesic effect)
-
Amnesia-the use of an amnestic
agent is common with midazolam (Versed) often employed.
Midazolam (Versed) belongs to the benzodiazepine category of
drugs
-
Reduction in secretion --
antisialagogue effect
-
Increase in gastric fluid pH
with a decrease in gastric fluid volume-these effects are
designed to reduce risk which may be associated with
aspiration
-
Reduction of autonomic
nervous system reflex responses-To accomplish this effect
sometimes antimuscarinic agents are used in as a consequence
surgical stimulation of muscarinic receptors are less likely
to provoke adverse cardiac effects (e.g. bradycardia,
arrhythmias)
-
Reduction in required
anesthetic amounts -- Premedication with sedative-hypnotic
agents and/or opioids to reduce the amount of anesthetic
required to achieve a given level of anesthesia. The
advantages may include more rapid emergence upon completion of
the case
-
Prophylaxis with respect to allergic reaction (e.g. antihistamines may be helpful)
-
Additional premedication issues:
-
Reduced cardiac activity (e.g.,
an anticholinergic drug such as atropine may prevent
bradycardia associated for example with surgical-induced
stimulation of muscarinic receptors). To manage cardiac vagal
activity, antimuscarinic agent should be administered DURING
surgery, just prior to the expected need or in response to
vagal stimulation
-
Reduction/avoidance of
postoperative nausea and vomiting-facilitated with I. V.
antiemetic drug administration JUST PRIOR to awakening (this
approach is probably better than waiting for symptom
developments and then treating the nausea)
-
Postoperative analgesia may be
best approached by use of IV opioids or neuraxial opioids JUST
PRIOR to symptom development-here administration may be
best provided just before awakening or just before a painful
surgical action
-
Circumstances in which
sedative-hypnotic (depressant) or some other pharmacological premedication would
be warranted:
-
Cardiac surgery
-
Cancer surgery
-
In the presence of pre-existing
pain
-
Regional anesthesia
-
Some circumstances in which
sedative-hypnotic (depressant) pharmacological premedication would
NOT be warranted:
-
In the hypovolemic patient
-
In the presence of significant,
severe pulmonary disease (additional respiratory depression
associated with sedative-hypnotics would be ill-advised)
-
Intracranial pathology
-
Reduced level of consciousness
-
Probably not in elderly
patients
-
Newborns (< 1 years of age)
-
Factors that influence the choice
those drugs for premedications and associated dosages
-
Whether the surgery is
classified as "inpatient" or "outpatient"
-
Whether the surgery is being
performed as an elective or emergency procedure
-
Concerns about the ability of
the patient to tolerate the drug
-
Patient age
and weight and
physical status
-
Anxiety level of the
patient-Recall that an anxious patient is likely to have
elevation of circulating catecholamines which may cause a
suboptimal cardiovascular preoperative state
-
Whether the patient has had an
adverse response to the particular medication during a
previous procedure-This consideration emphasizes how important
an adequate history or chart review is in deciding medication
choice.
Benzodiazepines
-
Overview:
-
Most commonly used sedative/anxiolytic
-
Anxiolytic effectiveness is
observed at dosages which do not result in cardiopulmonary
depression or excessive sedation
-
Certain benzodiazepines also
exhibit significant anterograde amnesia (amnesia subsequent to
drug administration).
-
Examples of these benzodiazepines
include midazolam (Versed) and lorazepam (Ativan).
-
These
agents may also cause, on predictably, some degree of
retrograde amnesia as well.
-
Benzodiazepines may also be
used the night before schedule surgery in management of
pre-surgical insomnia-- examples include lorazepam (Ativan),
temazepam (Restoril), and triazolam (Halcion)
-
Sometimes benzodiazepines used
pre-surgically can result in prolonged and excessive
sedation. Patients receiving lorazepam (Ativan) at high
dosages (total dose > 4 mg orally at 5 ug/kg) may be most
susceptible to this excessive sedation.
-
Intramuscular injection of
diazepam (Valium) may be painful because diazepam (Valium) is
dissolved in the irritating solvent propylene glycol;
intramuscular injections of midazolam (Versed) does not cause
local irritation since the chemical characteristics of
midazolam (Versed) do not require the use of propylene glycol
as a solvent (an aqueous solvent is used)
Adverse Effects: benzodiazepines
-
Major adverse effects
-
Inpatient considerations:
-
Outpatient considerations:
-
Factors/conditions which
increase likelihood of preoperative excessive sedation
associated with the use of benzodiazepines and other
sedative hypnotics:
-
Infancy, advanced age
(elderly patients), chronic debilitating disease or
malnutrition, pregnancy, renal dysfunction, hepatic
dysfunction, pulmonary dysfunction, adrenal insufficiency,
myasthenia gravis, myotonia, sickle cell disease, acute
drug/ethanol intoxication5.
3Comparisons: midazolam
(Versed), diazepam (Valium), and lorazepam (Ativan)
| |
Midazolam
(Versed) |
Diazepam
(Valium) |
Lorazepam
(Ativan) |
|
Dosage
(oral) |
0.3-0.5
mg/kg |
0.15-0.2
mg/kg |
0.015-0.03
mg/kg |
|
Time
to peak effect |
thirty
minutes-60 minutes |
1-1.5
hours |
2-4
hours |
|
Duration |
1-2
hours |
2-2.5
hours |
4-6
hours |
|
Elimination
halftime (time to reduce drug concentration by 50%) |
1-4
hours |
20-100
hours (includes active metabolites) |
8-24
hours |
|
Apparent
volume of distribution (Vd) |
1.1-1.7
L/kg |
0.7-1.7
L/kg |
0.8-1.3
L/kg |
|
Presence
of active metabolites |
yes,
but relatively weak in effect |
prominent |
none |
|
Metabolic
mechanism |
hydroxylation
and conjugation |
hydroxylation
and conjugation |
conjugation;
conjugation reactions are less likely to be affected by age or
the presence of hepatic disease |
|
Clearance |
6-11 ml/kg per
minute |
0.2-0.5 ml/kg
per minute |
0.7-1 ml/kg per
minute |
|
Lipid
solubility |
high |
high |
intermediate |
|
Effect
of age |
in
the elderly, midazolam (Versed) half-life may be increased by as
much as eight hours |
in
the elderly the half-life of diazepam (Valium) may be increased
by several days |
|
|
-
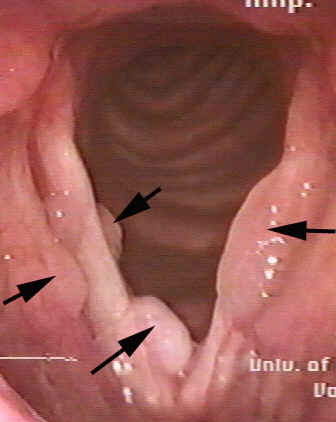
"The arrows point to multiple papilloma growths on the larynx caused by a viral infection. Permission to
reproduce
photo courtesy of the University of Pittsburgh Voice Center-
-
(Ed. note: This is a photograph that shows how laryngeal papillomatosis--RRP of the larynx--does not invariably
present with a traditional cauliflower-appearance.)"
|
|
Papillomatosis
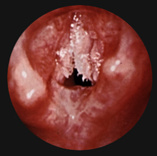
-
From On-Line Airway Atlas 2000,
John Sherry, II, M.D © 1999,2000
Epiglottis (with Abscess)
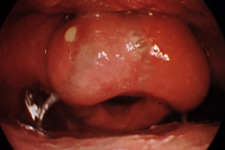
-
From On-Line Airway Atlas 2000 ,
John Sherry, II, M.D © 1999,2000
|
Benzodiazepine
pharmacology
|

Diazepam (Valium) |
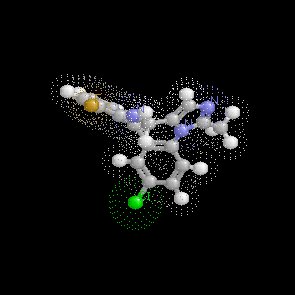
Midazolam (Versed) |
1Opioids
-
Overview
-
Advantages
for use in preoperative medication:
-
Absence
of myocardial depressant effects
-
Alleviate
the preoperative pain
-
Management
of discomfort associated with invasive monitor insertion
-
Management
of pain which may be associated with establishing regional
anesthetia
-
Preoperative
opioids may limit or eliminate the need for supplemental
analgesics during the early postoperative phase
-
Generally, in the absence of preoperative pain there may
be no compelling reason to include a narcotic for
preoperative anesthetic medication.
-
Commonly
used opioids for premedication
-
Contexts
for opioid administration:
-
Intramuscular: appropriate for
nitrous oxide-opioid anesthesia
-
Intravenous administration:
appropriately administered immediately before induction (fentanyl
(Sublimaze) is a good choice in this application)
-
Pain associated with
regional anesthesia or associated with invasive monitoring
catherization or even large intravenous lines may justify
treatment with preoperative opioids.
-
As would be expected
for many agents, dosage reduction may be required for the
elderly patient.
-
Elderly patients may have
reduced pain sensitivity that may exhibit an enhanced analgesic
response to the opioid
-
Occasionally preoperative opioids
are administered in advance of a nitrous oxide-opioid
anesthesia plan -- the rationale is that previous opioid
administration allows the anesthesia provider to gauge the
patients ensuing intraoperative opioid response.
-
For postoperative pain,
preoperative opioids may be employed; however, it is
probably preferable to either provide administration in to
recover room setting or perhaps most appropriately provide
IV opioids during the emergence
-
Preoperative opioid
administration may lower anesthetic requirements
-
For facemask induction,
opioids may be used in combination with other agents-in this
case opioid-mediated respiratory depression may decrease
ventilation during spontaneous breathing which will reduce
the rate of inhalational drug uptake. {the circumstance
might arise if for some reason intravenous induction agents
may not be used}
-
Adverse Effects:
-
Minimal cardiovascular effects
are noted, except for high-dose meperidine (Demerol)
-
Respiratory depression: associated with reduced responsiveness
to CO2 (medullary respiratory center
depression)
-
Orthostatic hypotension secondary to peripheral vascular smooth
muscle relaxation:
-
Opioids prevent the expected compensatory
peripheral vascular vasoconstriction.
-
This effect is in
addition to opioid- promoted histamine release that tends to
cause a hypotensive reaction.
-
The hypotensive response will be more
profound in patients who are hypovolemic.
-
Hypotensive reactions
can be avoided by ensuring that patients remained supine
following opioids (and other) premedication agents.
-
Nausea
and vomiting: These effects are frequently associated
with opioid administration, possibly occurring as a result of stimulation
of the medullary chemoreceptor trigger zone or vestibular
apparatus stimulation leading to motion sickness.
-
The likelihood of nausea
and vomiting may be reduced by placing the patient in a
recumbent position; however, the use of opioids because of
their tendency to cause nausea and vomiting perhaps should be
avoided in the same-day outpatient setting or if the
surgical procedure's themselves are likely to cause nausea
and vomiting {i.e. some gynecological and opthalmological
surgeries}
-
Delayed gastric emptying, which is associated with nausea
symptoms, has two important consequences-(1) altered absorption
rate for orally-administered agents and (2) and increased
risk of pulmonary aspiration
-
Opioids may also cause smooth muscle constriction (biliary spasm
{choledochododenal sphincter spasm, i.e. sphincter of Oddi}).
Manifestation consists of an upper right quadrant pain secondary
to smooth muscle constriction
-
Patients with
biliary tract disease should perhaps not receive opioids.
-
Also pain associated with biliary spasm, e.g. caused by an
opioid, may be difficult to distinguish from angina particularly
since pain from either angina or biliary spasm would be relieved
by smooth muscle relaxation due to sublingual nitroglycerin.
-
Opioid-induced pain, however, would be relieved by
administration of a pure opioid antagonist such as naloxone (Narcan)
or naltrexone (ReVia) or possibly glucagon. These drugs would not reverse true
anginal pain.
-
Meperidine (Demerol) is less
likely than morphine to cause biliary tract spasm.
-
Pruritis-probably secondary
to histamine release;
-
Accordingly opioids may cause flushing and
dizziness.
-
Since opioids are miotic
agents, pinpoint pupils may occur.
-
Specific agents:
-
Morphine:-
dosage (5-15 mg, IM Route of Administration)
-
Well absorbed following IM
administration
-
Time to onset: 15-30 minutes
with peak effect at about 45-90 minutes with total duration
of action as long as about four hours
-
Side reactions as noted for
the opioid group in general, including ventilation
depression; orthostatic hypotension as well as nausea and
vomiting secondary to effects on the chemoreceptor trigger
zone (CTZ) or on the vestibular apparatus
-
Reduction in GI motility
-
Preoperative use of morphine
reduces cardioacceleration associated with surgical
stimulation and volatile anesthetic agents
-
Meperidine
(Demerol) dosage: (50-150 mg, IM Route of Administration)
-
Less potent compared to
morphine (about 10% as potent)
-
Route of Administration: oral
or parenteral
-
Single dosage effect
duration: 2-4 hours with intramuscular injection providing a
variable time to peak effect and duration
-
Elimination: mainly through
hepatic metabolism
-
Cardiovascular effects:
positive chronotropic effect secondary to antimuscarinic
drug effects.
-
Fentanyl (Sublimaze):dosage-1-2
ug/kg intravenous for preoperative analgesia
-
Agonist-antagonist agents
-
These drugs, e.g. pentazocine
(Talwain), butorphanol (Stadol), nalbuphine exhibit reduced
respiratory depression compared to pure opioid agonists;
however, these drugs also have comparatively limited
analgesic effects.
-
These partial agonist,
given preoperatively, reduce the efficacy of pure opioid
agonist given postoperatively to control postoperative
pain. Partial agonist administration can in fact
limit or reverse analgesia caused by the presence of the
pure agonist
-
4Side effect incidence
following preoperative opioid administration: [1 hr following
dosage]-- original citation: Forest, w.H.,
Brown, B.W. et al.: "Subjective responses to six common
preoperative medications", Anesthesiology 47:241, 1977.
References:
-
1Preoperative Medication in
Basis of Anesthesia, 4th Edition, Stoelting, R.K. and Miller, R.,
p 119- 130, 2000)
-
Hobbs, W.R, Rall, T.W., and Verdoorn, T.A., Hypnotics and Sedatives;
Ethanol In, Goodman and Gillman's The Pharmacologial
Basis of Therapeutics,(Hardman, J.G, Limbird, L.E, Molinoff, P.B.,
Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,
1996, pp. 364-367.
-
3Sno E. White The Preoperative
Visit and Premedication in Clinical Anesthesia Practice pp.
576-583 (Robert Kirby and Nikolaus Gravenstein, eds) W.B.
Saunders Co., Philadelphia, 1994
-
4John R. Moyers
and Carla M. Vincent Preoperative Medication in Clinical Anethesia,
4th edition (Paul G. Barash, Bruce. F. Cullen, Robert K. Stoelting,
eds) Lippincott Williams and Wilkins, Philadelphia, PA, 2001
-
5Kathleen R.
Rosen and David A. Rosen, "Preoperative Medication" pp.
61-70 in Principles and Procedures in Anesthesiology (Philip
L. Liu, ed) J. B. Lipincott Company, Philadelphia, 1992
|