|
|
|
Medical Pharmacology Chapter 33-34: Anticancer Drugs
Antimetabolites
Purine Analogues: 6-Thiopurines:
6-Mercaptopurine (6-MP)
|
|
|
|
||
|
||
|
||
|
||
|
||
|
||
|
||
|
Summary
|
||
|
References
|
||
![]() 6-mercaptopurine is recognizes the first thiopurine analog determined to
show clinical effectiveness in treating cancer.
6-mercaptopurine is recognizes the first thiopurine analog determined to
show clinical effectiveness in treating cancer.
6-MP is mainly used in the treatment of childhood acute leukemia.
References
|
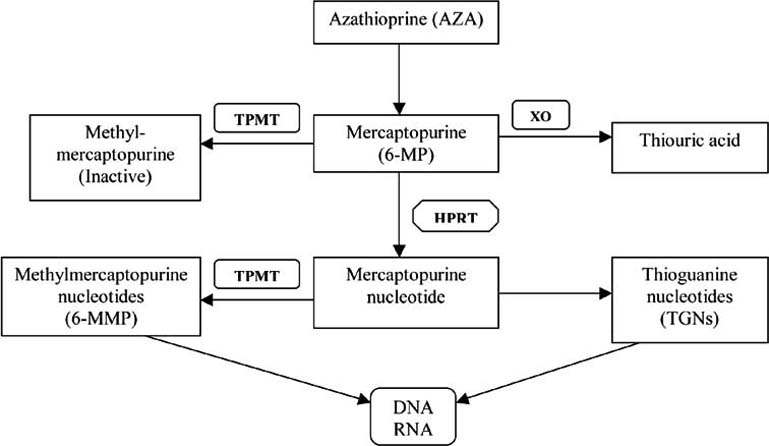
A related analog, azathioprine (Azasan) is available as an immunosuppressant drug.
6-mercaptopurine is a parent agent, a prodrug, which requires activation.
The active form, monophosphate nucleotide 6-thioinosinic acid, is formed by an enzyme catalyzed reaction.
|
|
|
The catalyzing enzyme is hypoxanthine-guanine phosphoribosyltransferase (HGPRT).
The monophosphate form is subsequently converted to the triphosphate form suitable for DNA or RNA incorporation.
An independent metabolic route is catalyzed by xanthine oxidase, resulting in inactive metabolites.9
Mercaptopurine is also susceptible to methylation at the sulfur resulting in metabolites that can be catabolized to respective nucleotides.
The methylation reaction-associated metabolites show relatively weak cytotoxic activity.
Furthermore, the enzyme that catalyzes this methylation reaction, thiopurine methyltransferase, exhibits genetic polymorphism with some patients showing very limited enzyme activity.9
![]() Patients
with deficiencies (partial or complete) in levels of thiopurine
methyltransferase are at elevated risk for significant toxicities.3
Patients
with deficiencies (partial or complete) in levels of thiopurine
methyltransferase are at elevated risk for significant toxicities.3
These toxicities are manifest as myelosuppression and gastrointestinal toxicity associated with both mucositis and diarrhea.3
The "Hichings and Elion" approach to drug development did not utilize the more typical trial-and-error method.
|
|
|
Instead George Hitchings (1905-1998) and Gertrude Elion (1918-1999) intentionally designed new molecules with specific molecular structures, and approach in contemporary science referred to as "rational drug design."
![]() Their
approach of rational drug design had by 1950 resulted in the synthesis
of two antimetabolites, diaminopurine and thioguanine.
Their
approach of rational drug design had by 1950 resulted in the synthesis
of two antimetabolites, diaminopurine and thioguanine.
These compounds are structural analogs of adenine and guanine and served as substrates for naturally occurring enzymes.
![]() Utilizing
the newly synthesized agents as substrates, the endogenous enzymes
created new purine structures which blocked DNA production.
Utilizing
the newly synthesized agents as substrates, the endogenous enzymes
created new purine structures which blocked DNA production.
These new drugs were notably effective for treating leukemia. Elion later extended this work by substitution of a sulfur atom for an oxygen atom, resulting in the synthesis of 6-mercaptopurine (6-MP).
6-MP also showed activity in treating leukemia.
Combination treatment involving 6-MP and other agents dramatically increased the likelihood of cure.
|
![]() The
mechanism of action of 6-mercaptopurine and 6-thioguanine involves
conversion catalyzed by hypoxanthine guanine phosphoribosyltransferase to
the ribonucleotides 6-thioGMP (6-thio-guanosine-5'-monophosphate) and
6-thio-IMP (6-thioinosine 5'-phosphate) (T-IMP).1
The
mechanism of action of 6-mercaptopurine and 6-thioguanine involves
conversion catalyzed by hypoxanthine guanine phosphoribosyltransferase to
the ribonucleotides 6-thioGMP (6-thio-guanosine-5'-monophosphate) and
6-thio-IMP (6-thioinosine 5'-phosphate) (T-IMP).1
Given that T-IMP is not a good substrate for guanylyl kinase which converts GMP to GDP.1
As a consequence, the intracellular concentration of T-IMP increases and T-IMP thus inhibits new formation of ribosyl-5-phosphate.
Also inhibited is conversion of IMP to adenine and guanine nucleotides.
An especially important site of inhibition involves reaction of glutamine and phosphoribosyl pyrophosphate (PRPP).
The reaction product, ribosyl-5-phosphate represents the first "committed" step in the de novo pathway.
![]() The 6-TG
nucleotide following DNA incorporation causes strand breaks as well as base
mispairing.
The 6-TG
nucleotide following DNA incorporation causes strand breaks as well as base
mispairing.
[6-MP is converted to an inactive metabolite, 6-thiouric acid, in a reaction catalyzed by xanthine oxidase.3
By contrast, 6-thioguanine (6-TG) is deaminated.
![]() The purine
analog allopurinol is a very effective xanthine oxidase inhibitor and can be
used in supportive care during acute leukemia treatment preventing
hyperuricemia associated with tumor cell lysis.]3
The purine
analog allopurinol is a very effective xanthine oxidase inhibitor and can be
used in supportive care during acute leukemia treatment preventing
hyperuricemia associated with tumor cell lysis.]3
Absorption, Disposition, Biotransformation, Excretion:1
Oral mercaptopurine is absorbed incompletely (with a range of 10% to about 50%). 1
Increased bioavailability is observed when mercaptopurine is administered in association with high-dose methotrexate.
By contrast, oral antibiotics or food tend to decrease absorption.
Following administration by the intravenous route of administration, the t1/2 of the drug is about one hour, as a result of degradation catalyzed by the enzymes, thiopurine methyltransferase and xanthine oxidase.
Mercaptopurine given orally is subject to notable hepatic first-pass metabolism catalyzed by xanthine oxidase.
![]() As a result
of the blood-brain barrier efflux transport system, mercaptopurine has
limited access to the brain.
As a result
of the blood-brain barrier efflux transport system, mercaptopurine has
limited access to the brain.
Metabolic pathways for mercaptopurine, in addition to hypoxanthine guanine phosphoribosyltransferase (HGPRT) include: 1
 |
|
(1) Methylation of the sulfhydryl group followed by oxidation of methylated derivatives.
![]() Thiopurine
methyltransferase (thiopurine S-methyltransferase, TPMT) exibits enzyme
activity influenced by inherited, polymorphic alleles.
Thiopurine
methyltransferase (thiopurine S-methyltransferase, TPMT) exibits enzyme
activity influenced by inherited, polymorphic alleles.
For example, some individuals of the Caucasian population (up to about 15%) exhibit reduced enzyme activity.
As measured by erythrocyte levels, erythrocyte TPMT appears associated with enhanced drug toxicity as well as reduce relapse risk.
![]() For
patients suffering autoimmune disease treated with mercaptopurine
and possessing polymorphic alleles, bone marrow aplasia and
life-threatening toxicities may occur.
For
patients suffering autoimmune disease treated with mercaptopurine
and possessing polymorphic alleles, bone marrow aplasia and
life-threatening toxicities may occur.
As a consequence, prior to treatment evaluation for the purpose of determining the presence of polymorphisms is appropriate for these individuals.
"Thiopurine S-methyltransferase (TPMT) is involved in the metabolism of all thiopurines and is one of the main enzymes that inactivates mercaptopurine.
"TPMT activity is inherited as a monogenic, co-dominant trait.
"More than 25 variants are known.
"Genetic testing is available for several TPMT variant alleles. Most commonly TPMT*2,*3A and *3C are tested for, which account for >90% of inactivating alleles."11
(2) Xanthine Oxidase: 1
Much of administered sulfate associated with administration of these thio-containing drugs may be recovered in the urine as an organic sulfate.
The other major pathway for mercaptopurine metabolism, noted above, is oxidation catalyzed by xanthine oxidase to an inactive metabolite, 6-thiourate.
![]() For
those patients receiving allopurinol, a xanthine oxidase
inhibitor often given to patients predisposed to gout,
6-mercaptopurine doses given orally should be reduced by about
75%.
For
those patients receiving allopurinol, a xanthine oxidase
inhibitor often given to patients predisposed to gout,
6-mercaptopurine doses given orally should be reduced by about
75%.
IV dosing of 6-mercaptopurine in these patients does not require dose changes.1
![]() Mechanisms of Drug Resistance:
Mechanisms of Drug Resistance:
Primary means for resistance to the action of 6-thiopurines may occur either by decreased levels of important cytotoxic nucleotide metabolites which can occur either by reduced synthesis or increased degradation.6
Some resistant cells exhibit complete/partial deficiency of hypoxanthine guanine phosphoribosyltransferase (HGPRT).
In these patients diagnosed with acute myelogenous leukemia (AML), analysis of clinical samples suggest increased levels of membrane-bound alkaline phosphatase or a conjugating enzyme, 6-thiopurine methyltransferase (TPMT).
Either of these increased enzyme levels cause a decrease in formation of the antineoplastic, cytotoxic thiopurine nucleotides.
Also, cellular drug resistance has been associated with reduced mismatch repair enzyme expression.6
![]() The most
frequently encountered mechanism of 6-mercaptopurine (6-MP) resistance
(based on in vitro studies) is either lack of activating enzyme HGPRT
(or deficiency in this enzyme) or enhanced alkaline phosphatase activity.1
The most
frequently encountered mechanism of 6-mercaptopurine (6-MP) resistance
(based on in vitro studies) is either lack of activating enzyme HGPRT
(or deficiency in this enzyme) or enhanced alkaline phosphatase activity.1
However, other mechanisms have been identified in these include:1
Reduced drug uptake or increased drug efflux by means of active transport mechanisms.
Changes in inhibition levels (allosteric-mediated) of ribosylamine-5-phosphate synthase.
Reduced cellular recognition of DNA breaks and mismatches secondary to loss of an element of the DNA mismatch repair system (the MSH6 component may be lost).1
GI (gastrointestinal) toxicity and myelosuppression represent the primary dose-related thiopurine toxicities.6
GI toxicity manifests as nausea/vomiting, diarrhea, anorexia and stomatitis.
Significant, excessive toxicity which can occur in TPMT-deficient individuals may be managed by a dosage reduction.
Thiopurine liver toxicity may occur in up to one-third of adult patients presenting usually as cholestatic jaundice.
In this setting, abnormally high hepatic transaminase enzyme activity may be observed.
Since thiopurine administration results in suppression of cell-mediated immunity, extended thiopurine administration may result in increased susceptibility of patients to bacterial and parasitic infections.6
6-mercaptopurine and azathioprine (a 6-MP derivative) administration increase the likelihood of:
Opportunistic infections
Hepatitis B reactivation
Fungal infection and
Pneumocystis pneumonia.
An increased likelihood of squamous cell skin malignancies has also been reported.
During the first pregnancy trimester, 6-MP is considered teratogenic.
Extended 6-mercaptopurine treatment durations for Crohn's disease appears associated with acute myelogenous leukemia (AML).