Nursing Pharmacology Chapter 35 Antibacterial Drugs
|
|
Bacterial cell wall structure
Multiple sites of inhibition by antibacterial agents
|
Inhibitors of Cell-Wall Synthesis
Overview
Penicillin G is bacteriocidal for sensitive strains, that is the agent itself can kill the bacteria as opposed to arrest growth (bacteriostatic)
The principal mechanism for penicillin bacteriocidal action is inhibition of cell wall synthesis with penicillin primarily affecting gram-positive organisms. Furthermore, for both the penicillins and cephalosporins bacteriocidal activity is dependent on actively growing bacteria which will be actively synthesizing new cell walls.
Penicillin is relatively nontoxic.
Disadvantages of Penicillin G
Disadvantages of penicillin G include the possibility of hypersensitivity reactions, a relatively short duration of action, and acid lability.
Particularly important concerns with the penicillins is sensitivity to ß-lactamases (penicillinases) which will limit effectiveness as well as their general lack of effectiveness against gram-negative organisms.
Not all penicillins exhibit acid lability. Acid stable penicillins include: carbenicillin (Geocillin), ampicillin (Principen, Omnipen), floxacillin, nafcillin (Nafcil, Unipen), dicloxacillin (Dynapen), oxacillin (generic) and penicillin V.
Penicillins which are beta-lactamase resistant (penicillinase resistant) as well as antipseudamonal* in their spectrum of action include: ampicillin (Principen, Omnipen), * piperacillin (Pipracil),*mezlocillin (Mezlin), *carbenicillin (Geocillin), amoxicillin (Amoxil Polymox), and *ticarcillin (Ticar).
Penicillin Structural Features and Requirements for Antibacterial Activity
|
|
|
Penicillin Binding Proteins (PBPs)
Penicillin-binding Proteins (PBPs) catalyze an important step in bacterial cell wall synthesis [a transpeptidase reaction which removes a terminal alanine in a crosslinking reaction with a nearby peptide].
One mechanism of penicillin antibacterial action is through binding to these proteins, thereby inhibiting their activity.
A Mechanism by which bacteria develop resistance to ß-Lactams is through alteration of penicillin-binding proteins (PBPs).
Resistance to beta-lactam antibiotics may be acquired either by mutation of existing PBP genes or, more importantly, by acquiring new PBP genes (e.g. staphlococcal resistance to methicillin) or by acquiring new "pieces" of PBP genes (e.g. pneumococcal, gonococcal and meningococcal resistance).
Chambers, H.F., Hadley, W. K. and Jawetz, E. Beta-Lactam and Other Inhibitors of Cell Wall Synthesis,in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p. 725.; Archer,G.L. and Polk, R.E. Treatment and Prophylaxis of Bacterial Infections, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, p. 859.
Activity Spectrum of Penicillins
Penicillins (Penicillin G): Activity Profile: Penicillins are effective against:
Gram posiitive organisms
Gram-negative cocci
Non-ß-lactamase producing anaerobes
Antistaphylococcal penicillins (nafcillin (Nafcil, Unipen)) are ß-lactamase resistant and are effective against:
Staphylococci
Streptococci
Extended Spectrum Agents (nafcillin (Nafcil, Unipen)), penicillinase sensitive, exhibit better activity against gram-negative organisms.
Archer,G.L. and Polk, R.E. Treatment and Prophylaxis of Bacterial Infections, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, p. 862-863; Chambers, H.F., Hadley, W. K. and Jawetz, E. Beta-Lactam and Other Inhibitors of Cell Wall Synthesis,in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p. 724.
Resistance: ß-Lactams
Most common among several mechanisms by which bacteria develop resistance to ß-Lactam antibiotics is by elaboration of the enzyme ß-lactamase, which hydrolyzes the ß-lactam ring.
ß-lactamase genes may be found in both gram-positive and gram-negative bactera.
Clavulanic acid and sulbactam, by binding to some ß-lactamases, can lessen resistance.
A second mechanism by which bacteria develop resistance to ß-Lactams is through alteration of penicillin-binding proteins (PBPs):
Either by mutation of existing PBP genes or, more importantly, by acquiring new PBP genes (e.g. staphlococcal resistance to methicillin) or by acquiring new "pieces" of PBP genes (e.g. pneumococcal, gonococcal and meningococcal resistance)
A third mechanism seen in gram-negative bacteria is due to alteration of genes that specify outer membrane proteins (porins) and reduce permeability to penicillins. (e.g. resistance of Enterbacteriaceae to some cephalosporins and that of Pseudomonas spp. to ureidopenicillins)
Multiple resistance mechanisms may be found in the same bacterial cell.
Archer,G.L. and Polk, R.E. Treatment and Prophylaxis of Bacterial Infections, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, p. 859.
Acid and ß-Lactamase Resistant Penicillins
![]() Acid Stable Penicillins include
Acid Stable Penicillins include
Carbenicillin
Indanyl
Ampicillin (Principen, Omnipen),
*Nafcillin (Nafcil, Unipen),
* Dicloxacillin (Dynapen)
*Cloxacillin (Cloxapen)
Oxacillin (generic)
Penicillin V (Pen-Vee K, Veetids).
*: ß-lactamase (Penicillinase resistant)
![]() Adverse Reactions
to Penicillins
Adverse Reactions
to Penicillins
The most common adverse reaction to penicillins are classified as hypersensitivity reactions. Furthermore, penicillins are the most common cause of drug allergy.
Hypersensitivity reactions from most common to least* are as follows:
Macropapular rash
Urticarial rash
Fever
Bronchospasm
Vasculitis
Serum sickness
Exfoliative dermatitis
Stevens-Johnson syndrome
Anaphylaxis
*Overall incidences is estimated to be between 0.7% to 10%.
![]() The most serious hypersensitivity
reactions caused by penicillin are angioedema and
anaphylaxis.
The most serious hypersensitivity
reactions caused by penicillin are angioedema and
anaphylaxis.
Angioedema is characterized by significant swelling of lips, tongue, face and periorbital tissues.
![]() Anaphylaxis places the patient in
the most immediate danger and may manifest as
sudden, severe hypotension and death.
Anaphylaxis places the patient in
the most immediate danger and may manifest as
sudden, severe hypotension and death.
Mandell, G.L. and Petri, W. A. Antimicrobial Agents: Penicillins, Cephalosporins, and other ß-Lactam Antibiotics.,In, Goodman and Gillman's The Pharmacologial Basis of Therapeutics, (Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996, pp.1086-1088)
Penicillin (Penicillin G) Effective Against:
Staphylococci-non beta-lactamase producing
streptococci non-beta-lactamase producing
Bacillus anthracis
Enterococci
Meningococci, Actinomyces
Spirochetes
Clostridium
Gram-positive rods.
Penicillins may be sensitive to beta-lactamase producing bacteria.
Those penicillins resistant to beta-lactamase producing staphylococcal strains include:
Methicillin (Staphcillin)
Nafcillin (Nafcil, Unipen) and
Certain isoxazolyl penicillins such as
Oxacillin (generic)
Cloxacillin (Cloxapen), and
Dicloxacillin (Dynapen).
![]() All penicillins (excepting semisynthetic, penicillinase-resistant antistaphylococcal agents) can be
hydrolyzed by ß-lactamases enzymes and will not be
efficacious against bacterial strains that produce this
enzyme.
All penicillins (excepting semisynthetic, penicillinase-resistant antistaphylococcal agents) can be
hydrolyzed by ß-lactamases enzymes and will not be
efficacious against bacterial strains that produce this
enzyme.
Clinical Indications for penicillins resistant to beta-lactamase producing staphylococcal strains.
The primary indication would of course the infection by beta-lactamase producing staphylococcal organisms.
However, other susceptible bacteria include penicillins susceptible strains of streptococci and pneumococci.
These drugs however all are enacted against enterococci, anaerobic bacteria, gram-negative cocci and rods.
Chambers, H.F., Hadley, W. K. and Jawetz, E. Beta-Lactam and Other Inhibitors of Cell Wall Synthesis,in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p. 729.
Cephalosporins are similar to penicillins in terms of mechanism of action, chemical structure, and toxicities.
By targeting bacterial cell wall transpeptidases and penicillin binding proteins (PBPs), cephalosporins cause cells wall lysis, which is the basis of bacteriocidal activity for susceptible bacteria.
Although many (most) bacteria contain PBPs, cephalosporin antibiotics are not effective against all bacteria as a result of resistance.
Cephalosporins and their Spectrum of Pharmacological Action
First-generation agents (Cephalothin and cefazolin) exhibit good activity against gram-positive bacteria, but less activity against gram negative organisms.
Most gram-positive cocci are susceptible to first-generation cephalosporins-(not including enterococci and methicillin-resistant staph)
Most oral cavity anaerobes are sensitive. However, the B. fragilis group is resistant.
Good activity against Moraxella catarrhalis, E. coli, K. pneumoniae and Proteus mirabilis.
Second-generation agents include. cefoxitin (Mefoxin), cefotetan (Cefotan), cefmetazole(Zefazone)).
Second-generation drugs exhibit somewhat enhanced activity against gram negative organisms, but much less enhancement compared to third generation agents.
Third-generation agents: (e.g. cefotaxime (Claforan), ceftriaxone (Rocephin), ceftazidime (Fortax, Taxidime, Tazicef)):
Third-generation cephalosporins are less active than First generation agents against gram-positive cocci
However, these drugs are much more active against Enterobacteriaceae, including those that produce ß-lactamase.
Fourth-generation agents (e.g. cefepime (Maxipime)):
Fourth generation cephalosporins are generally similar to third generation drugs, although the fourth generation drugs exhibit increased resistance to beta-lactamase-producing bacteria.
|
Klebsiella pneumoniae
|
Organisms susceptible to Cephalosporins
First Generation: Cefazolin (Ancef): Streptococci (except for penicillin-resistant strains)
|
|
First Generation: Cefazolin (Ancef): Staphylococcus aureus (except for methicillin-resistant strains)
|
photo credit: Kenneth Todar University of Wisconsin Department of Bacteriology
3 Timothy Foster "Staphylococcus" in Medical Microbiology (4th edition) edited by Samuel Baron, M.D., The University of Texas Medical Branch, |
Second Generation: Cefuroxime (Ceftin), Cefaclor (Ceclor):
Klebsiella, Haemophilus influenzae, E.coli, Moraxella catarrhalis and Proteus mirabilis
Third-generation: Cefotaxime (Claforan), Ceftriaxone (Rocephin), Ceftazidime (Ceptaz):
Enterobacteriaceae, Pseudomonas aeruginosa, Serratia, Neisseria gonorrhoeae; activity for Staph. aureus and Strept. pyogenes similar to first generation agents.
Mandell, G.L. and Petri, W. A. Antimicrobial Agents: Penicillins, Cephalosporins, and other ß-Lactam Antibiotics.,In, Goodman and Gillman's The Pharmacologial Basis of Therapeutics,(Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996, pp.1089-1092
More about Cephalosporins
First Generation Cephalosporins are rarely a drug of choice.
However, these agents are very active against gram-positive cocci, but are not active against methicillin (Staphcillin)-resistant isolates of staphylococci.
First-generation agents are excreted by glomerular filtration and tubular secretion which may be blocked by probenecid (Benemid).
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 732-733.
Second Generation Cephalosporins exhibit activity against gram-positive cocci with an extended gram-negative spectrum compared to first-generation agents.
Second generation drugs are active against beta-lactamase producing H.influenzae. Furthermore, good activity is exhibited against anaerobes which is a particularly useful characteristic in mixed infections such as peritonitis.
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, p. 734.
Third Generation Cephalosporins are generally more active against gram-negative organisms (except for the drug cefoperazone (Cefobid)). Some members of this group have enhanced ability to cross the blood-brain barrier.
Third-generation drugs tend to exhibit activity against Citrobacter, Serratia marcescens and Providencia and ß-lactamase producing Haemophilus and Neisseria.
Third generation cephalosporins are effective in treating a large variety of infections resistant to many other drugs
Ceftriaxone (Rocephin) and and cefixime (Suprax) are first-line antibiotics for treating gonorrhea.
Third generation agents cross the blood brain barrier and are effective in treating menningitis caused by pneumococci, meningococci, H. influenzae and susceptible gram negative rods (not by Listeria monocytogenes)
Ceftriaxone (Rocephin) and cefotaxime (Claforan) are the most active cephalosporins against penicillin-resistant pneumococci.
Third generation agents may not be effective in treating menningitis caused by highly penicillin-resistant strains and treatment may require addition of vancomycin (Vancocin) or rifampin (Rimactane)
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 734-735.
Specific First Generation Cephalosporin Drugs
First generation cephalosporins include: cephalexin (Keflex), cephradine (Velosef), cephalothin (Keflin), cefadroxil (Duricef, Ultracef),and cephapirin (Cefadyl)
First generation cephalosporins are administered orally an exhibit a fairly broad spectrum of action while being relatively nontoxic.
These agents appear suitable for treatment of urinary tract infections (UTI), cellulitis or soft tissue abscess.
Oral cephalosporins not indicated for serious systemic infections.
Review and Overview: Second Generation Cephalosporins
Second generation agents are active against gram-positive cocci an exhibit an extended gram-negative spectrum compared to first generation drugs.
Second generation drugs are generally effective against beta-lactamase reducing H.influenzae.
They exhibit good activity against anaerobes and are effective in mixed-infections, as an example, peritonitis.
Examples of second generation cephalosporins:
Cefaclor (Ceclor), cefamandole (Mandol), cefaclor (Ceclor), and cefonicid (Monocid).
Cefuroxime (Zinacef, Ceftin) is effective in community-acquired pneumonia or take your leave the causative organism may be beta-lactamase producing H.influenzae or Klebsiella pneumoniae. Cefuroxime (Zinacef, Ceftin) is the only second-generation drug across the blood-brain barrier, although third-generation agents such as ceftriaxone (Rocephin) or cefotaxime (Claforan) or more effective in managing meningitis.
Cefprozil (Cefzil) ceforanide (Precef).
Cefmetazole (Zefazone) cefotetan (Cefotan) and Cefoxitin (Mefoxin) are effective in mixed anaerobic infections due to activity against anaerobes (e.g. B. fragilis).
Review and Overview: Third Generation Cephalosporins
Generally, third-generation drugs are more active against gram-negative microbes (except cefoperazone) and exhibit enhanced ability (in some cases) to traverse the blood brain barrier.
These agents areActive against Citrobacter, Serratia marcescens and Providencia and ß-lactamase producing Haemophilus and Neisseria.
Third generation cephalosporins are effective in treating a large variety of infections resistant to many other drugs.
Ceftriaxone (Rocephin) and and cefixime (Suprax) are first-line antibiotics for treating gonorrhea.
Third generation agents cross the blood brain barrier and are effective in treating menningitis--caused by pneumococci, meningococci, H. influenzae and susceptible gram negative rods (not by Listeria monocytogenes)
Ceftriaxone (Rocephin) and cefotaxime (Claforan) most active cephalosporins against penicillin-resistant pneumococci.
Third generation agents may not be effective in treating menningitis caused by highly penicillin-resistant strains and treatment may require addition of vancomycin (Vancocin) or rifampin (Rimactane)
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 734-735.
Examples of third generation cephalosporins
Ceftazidime, Cefoperazone are effective against P. aeruginosa. (Third-generation cephalosporins are hydrolyzed by enterobacter chromosomal ß-lactamase)
Cefotaxime (Claforan)
Ceftizoxime (Cefizox)
Ceftriaxone, Cefixime
Drugs of choice in treatment of gonorrhea since many isolates of N gonorrhoeae are penicillin resistant
Ceftriaxone (Rocephin)/cefixime should not be used to treat Enterobacter infections due to the likelihood of resistance emergence.
Proxetil
Cefibute
Moxalactam
Cefepime, although classified as a fourth-generation agent, exhibits many properties of third-generation cephalosporins. Cefepime (Maxipime) is somewhat more resistant to hydrolysis by beta-lactamases and exhibits activity against certain beta-lactamases which inactivate many third-generation drugs.
Cefepime (Maxipime) exhibits activity against most penicillin-resistant strains of streptococci and has been considered effective in management of Enterobacter infections. At this agent also exhibits effectiveness against Staphylococcus aureus, Staphylococcus pneumoniae, Enterobacteriaceae and P. aeruginosa.
Generally, cefepime (Maxipime) may be considered clinically comparable to most third-generation cephalosporins.
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 732-736;Chambers, H.F., Beta-Lactam Antibiotics and Other Inhibitors of Cell Wall Synthesis in Basic and Clinical Pharmacology, (Katzung, B. G., ed), Appleton-Lange, 2001, p. 766.
Other ß-lactam containing antibacterials
Aztreonam (Azactan)
Aztreonam (Azactan) is a synthetic monobactam antibiotic, having a moncyclic, rather than a bicyclic nucleus.
This agent inhibits synthesis of bacterial cell wall by high-affinity binding to penicillin-binding protein (PBP3 ) which is found primarily in aerobic, Gram-negative microbes.
Aztreonam (Azactan) is highly resistant to ß-lactamases.
Spectrum of activity includes aerobic, Gram-negative bacterial and is similar in activity to aminoglycosides without causing ototoxicity or nephrotoxicity.
Aztreonam (Azactan) is effective in treating Gram-negative urinary tract infections, lower respiratory tract, skin, intraabdominal, gynecologic infections and septicemia.
This drug may be used in combination with other antibiotics which are active against Gram-positive microbes and anaerobes in mixed infections.
Contraindications for Aztreonam (Azactan): safe use during pregnancy (category B), in nursing women, infants and children has not established.
Cautious use: hypersensitivity history to penicillin, cephalosporins; impaired renal or liver function.
Aztreonam (Azactan) exhibits activity against Hemophilus influenzae, Pseudomonas aeruginosa, Neisseria gonorrhoeae and Enterobacteriacea including most isolates of E . coli, Enterobacter, Klebsiella, Proteus, Providencia, Shigella, Salmonella, and Serratia.
Shannon, M.T., Wilson, B.A., Stang, C. L. In, Govoni and Hayes 8th Edition: Drugs and Nursing Implications Appleton and Lange, 1995, pp. 166-167.
Imipenem Premaxin, Meropenem
Combination of imipenem, a ß-lactam antibiotic, and cilastin which inhibits dipeptidase enzyme degradation of imipenem. Without cilastin renal dehydropeptidases inactivate the drug which results in low urinary tract concentrations.
Imipenem inhibits bacterial cell wall mucopeptide synthesis and is bacteriocidal.
very wide spectrum among the ß-lactams, providing good coverage of gram-negative rods, gram-positive bacteria, and anaerobes.
ß-lactamase resistant.
Not Effective in treating: Enterococcus faecium, methicillin-resistant strains of staphylococci, Claostridium difficile, Burkholderia cepacia and Stenotrophomonas maltophilia.
Synergistic actions with aminoglycoside antibiotics against some strains of Pseudomonas aeruginosa. Combination with an aminoglycoside is recommended because of Pseudomonas rapidly develops resistance to imipenem.
Agent of choice for treating Enterobacter infections.
Meropenem has somewhat great antibacterial effects against gram-negative aerobes and slightly less activity against gram-positive organisms.
Meropenem is less seizure producing compared to imipenem.
Effective in treating these infections
Urinary tract
Lower respiratory tract
Bone
Joint
Skin
Intra-abdominal
Gynecological
Mixed infections
Endocarditis
Bacterial septicemia
Contraindications:
Contraindicated: hypersensitive patients
Safe use in pregnancy (category C) or in children <12 not established.
Caution use: nursing mothers
Cautious use: patient with CNS disorders including seizures, brain lesions; renal impairment
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, p. 737..;Shannon, M.T., Wilson, B.A., Stang, C. L. In, Govoni and Hayes 8th Edition: Drugs and Nursing Implications Appleton and Lange, 1995, pp. 614-615.
Clavulanic acid, Sulbactam, Tazobactam
Clavulanic acid, sulbactam and tazobactam are potent inhibitors of many bacterial ß-lactamases.
These agents are given together with hydrolyzable penicillins to protect them from inactivation.
Most effective against plasmid-encoded beta-lactamases including those produced by:
Staphylococci
H. influenzae
N. gonorrhoeae
Salmonella
Shigella
E. coli
K. pneumoniae
Not effective inhibitors of inducible chromosomal ß-lactamases which are produced by Enterobacter, Citrobacter, Serratia, Pseudomonas.
These similar drugs are given in fixed combination with specific penicillins which determines the antibacterial spectrum.
The ß-lactamase inhibitors can extend the spectrum of an antibiotic, e.g. ampicillin in combination with sulbactam is effective against ß-lactamase producing S. aureus and H. influenzae.
Effectiveness is dependent upon the variant of ß-lactamase enzyme produced.
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 736-737.
Other Inhibitors of Cell-Wall Synthesis
Vancomycin
Vancomycin, a glycopeptide, is active only against gram-positive bacteria, especially staphylococci {one exception is that it is active against Flavobacterium}
Vacomycin is an inhibitor of bacterial cell wall synthesis by preventing peptidoglycan elongation and cross-linking.
Critical resistance to the antibacterial action of vancomycin is due to a modification of its peptidoglycan binding site, a modification that reduces binding affinity.
Vancomycin is bacteriocidal for gram-positive bacteria including ß-lactamase producing staphylococci and those resistant to nafcillin and methicillin.
Vancomycin kills only dividing cells and relatively slowly.
Vancomycin acts synergistically with gentamicin and streptomycin (aminoglycosides) against E. faecium and E. faecalis isolates not resistant to aminoglycosides.
Major Clinical Use
Sepsis
Endocarditis due to methicillin resistant staphylococci
Methicillin-susceptible Staph isolates would likely be more effectively treated with methicillin than vancomycin.
Treatment alternative enterococcal endocarditis.: Vancomycin with gentamycin: for patient allergic to penicillin.
Vancomycin incombination with cefotaxime, ceftriaxone or rifampim: appropriate for treatment of mennigitis when the suspected infecting agent is thought/known to be highly penicillin resistant.
Bacitracin
Bacitracin is a cyclic peptide mixture that is active against gram-positive microbes.
Bacitracin inhibits cell wall formation by interfering with peptidoglycan transfer to the developing cell wall and exhibits no cross-resistance between bacitracin and other antimicrobials.
Due to systemic toxicity, bacitracin is limited to topical use.
Major Clinical Use
Alone or in combination with polymyxin or neomycin: treatment of mixed skin, wound or mucous membrane infections.
Adverse Effects
Significant nephrotoxicity with systemic administration
Cycloserine
Cycloserine, a structural analog of D-alanine, inhibits both Gram-positive and Gram-negative bacteria.
Mechanism of action is inhibition of D-alanine incorporation into peptidoglycan by inhibiting alanine racemase (which converts L-alanine to D-alanine) and D-alanyl-D-analanine ligase
Major Clinical Use
Used almost exclusively for treating tuberculosis caused by M. tuberculosis isolates resistant to primary drugs.
Adverse Effects
CNS toxicity at higher than clinical doses
Chambers, H.F., Hadley, W. K. and Jawetz, E. Introduction to Antimicrobial Agents in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp. 739-740
Membrane-Active Agents: Mechanisms of action of polymixin and gramicidin antibacterial action and Clinical uses of these agents
Polymixins
Polymixins (polymixin E) are amphipathic (containing lipophilic and lipophobic groups) basic peptides which exhibit activity against gram-negative bacteria.
They are bacteriocidal for many gram-negative rods including Pseudomonas.
Polymixins disrupt bacterial cell membranes through strong interactions with phospholipid components.
Gram-positive bacteria, Proteus, Neisseria are resistant to polymixins.
Polymixin B sulfate used topically for treatment of external otitis and corneal ulcers due to Pseudomonas aeruginosa.
Systemic use of polymixins not recommended becasue of poor tissue distribution, significant nephrotoxicity and neurotoxicity and the availability of more effective other antibacterial drugs.
Polymixin E is active against:
Pseudomonas aeruginosa
Escherichia coli
Enterobacter
Klebsiella
Clinical Applications of Polymixin B
Skin, mucous membrane, eye and ear infections (for sensitive organism).
For example, external otitis (Pseudomonas) or corneal ulcers (Pseudomonas aeruginosa
Sometimes used by aerosol as an adjunct to other antibiotics in difficult cases of Pseudomonas pneumonia.
Chambers, H.F.and Hadley, W. K. Micellaneous Antimicrobial Agents: Disinfectants, Antiseptics adn Sterilants, in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, pp 803-804
Robertson, D.B, and Maibach, H.I. Dermatologic Pharmacology , in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p 1000
Kapusnik-Uner, J.E., Sande, M.A. and Chambers,J.F. Antimicrobial agents: Tetracyclines, Chloramphenicol, Erythromycine, and Miscellaneous Antibacterial Agents, In, Goodman and Gillman's The Pharmacologial Basis of Therapeutics,(Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) The McGraw-Hill Companies, Inc.,1996, pp.1143-1144.
Gramicidin
Gramicidin: peptide antibiotic which alters membrane permeability-effective against gram-positive organisms
Gramicidin may be used in combination with neomycin, polymyxin B or both.
Available only for topical usage
Systemic toxicity
Gramicidin Active Against:
Streptococci
Pneumococci
Staphylococci
Most anaerobic cocci
Neisseriae
Tetanus bacilli
Diphtheria bacilli
Robertson, D.B, and Maibach, H.I. Dermatologic Pharmacology , in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p 1000.
Mechanistic Comparisons: Membrane Active Agents vs. Inhibitors of Cell-Wall Synthesis
Polymixin B
Polymixins (polymixin E): basic peptides which are amphipathic (containing lipophilic and lipophobic groups)
Disrupt bacterial cell membranes through strong interactions with phospholipid components.
Inhibitors of Cell Wall Synthesis
Penicillin-binding Proteins (PBPs) catalyze an important step in bacterial cell wall synthesis [a transpeptidase reaction which removes a terminal alanine in a crosslinking reaction with a nearby peptide].
One mechanism of penicillin antibacterial action is through binding to these proteins, thereby inhibiting their activity.
Inhibitors of protein synthesis (IPS)
Rationale for targeting of bacterial protein synthesis
Relationships between mechanism and therapeutic/adverse effects
Aminoglycosides: Mechanisms of action for aminoglycosides
Chloramphenicol: (Chloromycetin)
Chloramphenicol, macrolides, and clindamycin (Cleocin) bind to bacterial ribosomal RNA (50S subunit of 70S ribosomal RNA)
Chloramphenicol blocks binding of charged tRNA to its binding site on the ribosomal RNA-mRNA complex.
As a result, transpeptidation cannot occur and the peptide is not transfered to the amino acid acceptor.
Protein synthesis stops.
Macrolides and clindamycin (Cleocin) block movement of peptidyl tRNA from acceptor to donor site.
As a result, the next, incoming tRNA cannot bind to the still occupied acceptor site.
Protein synthesis stops.
Tetracycline binds to 40S ribosomal RNA, blocking association of amino acid-charged tRNA with its acceptor site on the ribosomal mRNA complex.
Protein synthesis stops.
Susceptibility differences between bacterial and mammalian cells
Mammalian 80S ribosomal RNA does not bind chloramphenicol.
However, mammalian mitochondrial ribosomal RNA (70S) does bind chloramphenicol.
Chloramphenicol (Chloromycetin) dose-related bone marrow suppression may be due to drug's effect on mitochondrial ribosomes
Tetracycline inhibits mammalian cell protein synthesis, but an active efflux system may prevent intracellular drug concentrations from reaching toxic levels.
Protein synthesis inhibition is probably due to binding to 30S ribosomal proteins.
Detailed analysis of streptomycin suggest three specific protein synthesis inhibition mechanisms:
Interference with "initiation complex" of peptide formation
Causing misreading of mRNA which results in incorrect amino acid incorporation
Promotion of polysomal dissociation into nonfunctional monosome.
These combined effects, occurring at the same time, are probably responsibile for aminoglycoside bacteriocidal properties.
Spectrum of activity and clinical uses:
Aminoglycosides: gram-negative enteric bacteria especially if the microbe is suspected to be a drug-resistant isolate or sepsis may be present.
Nearly always used in combination with a ß-lactam to extend coverage to possibly gram-positive microbes.
Aminoglycosides and ß-lactams are synergistic.
Penicillin-aminoglycoside combinations:
bacteriocidal in enterococcal endocarditis reduces therapy duration for viridans streptococcal and staphylococcal endocarditis.
![]() Classic adverse
effects of aminoglycosides
Classic adverse
effects of aminoglycosides
Aminoglycosides are ototoxic and nephrotoxic.
Aminoglycoside in patients receiving a loop diuretic (furosemide) or other nephrotoxic antibiotics (vancomycin (Vancocin) or amphotericin B (Fungizone)) worsens renal toxicity.
Ototoxicity manifests as: tinnitus, high-frequency hearing loss or as vestibular damage: vertigo ataxia.
Reduced creating clearance and increasing serum creatinine are associated with aminoglycoside-induced renal toxicity. First indications of aminoglycoside renal toxicity may be increased "trough" drug concentrations, reflecting decreasing renal drug clearance.
Very high aminoglycoside doses produce neuromuscular blockade (paralysis) which is reversible in early stages by calcium infusion or by neostigmine.
|
Most ototoxic |
Most toxic to the vestibular system |
|
|
Chambers, H.F., Hadley, W. K. and Jawetz, E. Aminoglycosides and Spectinomycin,in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, pp. 753-754
Specific drugs
Streptomycin
Streptomycin: main use: second-line treatment for tuberculosis
Used only in combination with other antimicrobials (otherwise rapid emergence of resistance)
In combination with oral tetracycline, i.m. streptomycin may be used in treating:
Plague
Tularemia,
Bucellosis.
In combination with penicillin:
Treatment for enterococcal endocarditis
Vridans streptococcal endocarditis (two-week regimen)
Adverse Reactions
Fever
Rash (hypersensitivity)
Most serious toxic effect: vestibular toxicity which tends to be irreversible.
Treptomycin administration during pregnancy may result in deafness in the newborn.
Gentamicin (Garamycin)
Gentamicin (Garamycin): effective against gram-positive and gram-negative microbes
Active alone but shows synergism with ß-lactam antimicrobials in managing:
Pseudomonas
Proteus
Enterobacter
Klebsiella
Serratia
Stenotrophomonas
Other gram-negative rods but no activity against anaerobes.
![]() Primary
clinical use: Treatment of
severe gram-negative bacterial infections
(sepsis/pneumonia) when the bacteria is likely
resistant to other antibiotics.
Primary
clinical use: Treatment of
severe gram-negative bacterial infections
(sepsis/pneumonia) when the bacteria is likely
resistant to other antibiotics.
The combination of gentamicin and a cephalosporin or penicillin may be life-saving in the immunocompromised patient.
Gentamicin + penicillin G: viridans streptococcal endocarditis
Gentamicin + nafcillin (Nafcil, Unipen) in some cases of staphylococcal endocarditis.
Gentamicin should not be used as a single agent due to rapid development of resistance.
Aminoglycosides should not be used as single therapy in pneumonia due to poor tissue penetration.
Nephrotoxicity: requires serum gentamicin monitoring if administration exceeds a few days.
Adverse Reactions: nephrotoxicity, deafness, vestibular toxicity which is often irreversible.
Tobramycin (Nebcin)
Antibacterial spectrum of action similar to gentamicin.
Some cross-resistance possible
Nearly identical pharmacokinetic profile
Similar antimicrobial spectum to gentamicin.
Adverse Reactions
Nephrotoxicity
Deafness
Vestibular toxicity which tends to be irreversible.
Amikacin (Amikin)
Amikacin: semisynthetic derivative of kanamycin, but less toxic.
Amikacin may be used against microbes resistant to:
gentamicin or tobramycin because it is resistant to enzymes which inactivate those agents.
Often effective in treating multi-drug resistant strains of Mycobacterium tuberculosis.
Kanamycin resistant isolates are likely to exhibit cross-resistance to amikacin.
Amikacin (Amikin) is ototoxic (auditory component especially) and nephrotoxic, as are all aminoglycosides.
Kanamycin and Neomycin
Kanamycin and Neomycin: Active against gram-positive, gram-negative and some mycobacteria.
Pseudomonas and streptococci: resistant
Mechanisms of action and resistance follow that of other aminoglycosides.
Cross-resistance between these agents and kanamycin and neomycin
Neomycin: topical and oral use only due to toxicity associated with parenteral administration.
Neomycin use: given prior to elective bowel surgery, reducing aerobic bowel flora.
Ototoxicity (auditory) and nephrotoxicity.
Spectinomycin (Trobicin)
Spectinomycin: structurally-related to aminoglycosides.
Used almost exclusively to treat gonorrhea resistant to other drugs or if the patient is allergic to penicillin.
No cross-resistance between spectinomycin and other drugs used to treat gonorrhea
The dependency of therapeutic and toxic effects on pharmacokinetics
Aminoglycosides are poorly absorbed from the G.I. tract
Most of the oral dose is excreted directly. Aminoglycosides are usually administered intravenously (i.v).
Highly polar molecules, aminoglycosides do not penetrate the CNS or eye.
In menningitis with attendant inflammation, cerebral spinal fluid levels may reach 20% of plasma concentration.
Higher concentration requires directly intrathecal or intraventricular administration.
Tissue drug levels are generally low, except in the renal cortex.
Renal aminoglycosides clearance rates are directly proportion to creatinine clearance rates.
Many factors (age, gender) influence the relationship between serum creatinine levels and creatinine clearance. Reliance on estimated creatinine clearance is appropriate in determining aminoglycoside dosage in a patient.
In renal insufficiency, care must be used to avoid toxicity due to drug accumulation.
Development of resistance to aminoglycosides
Most common mechanism of resistance is antibiotic inactivation by enzyme-mediated covalent modification which results in phosphate, adenyl or acetyl group transfer.
Aminoglycoside-modifying enzymes are plasmid localized.
The modified antibiotic is also less active because of decreased transport and decreased binding to the ribosomal target site
Aminoglycoside-modifying enzymes have been found in both gram-negative and gram-positive bacteria.
Tetracyclines, macrolides, chloramphenicol, clindamycin, spectinomycin
Inhibitors of folate-dependent pathways
Production and use of folate derivatives in bacterial systems
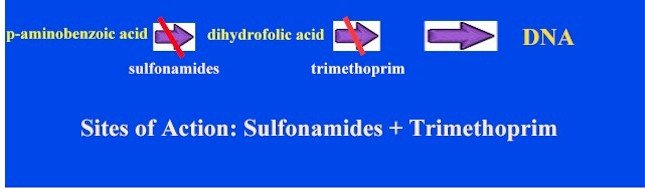
Certain microbes require para-aminobenzoic acid (PABA) in order to synthesize dihydrofolic acid which is required to produce purines and ultimately nucleic acids.
Sulfonamides,chemical analogs of PABA, are competitive inhibitors of dihydropteroate synthetase.
Sulfonamides therefore are reversible inhibitors of folic acid synthesis and bacterostatic not bacteriocidal.
Sulfonamides
Mechanism of action of sulfonamides
Certain microbes require p-aminobenzoic acid (PABA) in order to synthesize dihydrofolic acid which is required to produce purines and ultimately nucleic acids.
Sulfonamides,chemical analogs of PABA, are competitive inhibitors of dihydropteroate synthetase.
Sulfonamides therefore are reversible inhibitors of folic acid synthesis and bacterostatic not bacteriocidal.
Trimethoprim
Trimethoprim
(generic) mechanism of action
Trimethoprim is
an inhibitor of bacterial dihydrofolic acid reductase.
Pyrimethamine
(Daraprim) is an excellent inhibitor of
dihydrofolic acid reductase in protozoa
These reductases are required for
the synthesis of purines and hence DNA.
Inhibition
of these enzymes are responsible for
bacteriostatic and bacteriocidal activities.
When
trimethoprim or pyrimethamine is combined with sulfonamides (sulfamethoxazole)
there is sequential blocking of the biosynthetic
pathway leading to drug synergism and enhanced
antimicrobial activity. (see figure below)
Resistance to trimethoprim:
usually by plasmid encoded trimethoprim-resistant
dihydrofolate reductases.
Trimethoprim typically used orally
often in combination with sulfamethoxazole, a
sulfonamide with a similar half-life.
Archer,G.L. and Polk, R.E.
Treatment and Prophylaxis of Bacterial Infections, In
Harrison's Principles of Internal Medicine 14th edition, (Isselbacher,
K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper,
D.L., eds) McGraw-Hill, Inc
(Health Professions Division), 1998, p. 859. Chambers, H.F., Hadley, W. K.
and Jawetz, E. Aminoglycosides and Spectinomycin,in Basic
and Clinical Pharmacology,(Katzung, B. G., ed)
Appleton-Lange, 1998, p. 752 Clinical Uses
Oral trimethoprim: Acute urinary
tract infections
Oral
trimethoprim-sulfamethoxazole (Bactrim)
combination: Pneumocystis carinii
pneumonia, shigellosis,systemic
Salmonella infection, some nontuberculous
mycobacterial infections.
Respiratory tract pathogens:
pneumococcus, Haemophilus, Moraxella
catarrhalis, Klebsiella
pneumoniae
By I.V.
administration trimethoprim - sulfamethoxazole: agent
of choice for moderately severe to severe
infections with
Pneumocystis carinii
pneumonia, especially in patients with
HIV. May be used for
gram-negative sepsis
Trimethoprim adverse effects
referable to antifolate properties: megaloblastic
anemia, leukopenia granulocytopenia
(avoided by coadminstration of folinic
acid)
Combination of
Trimethoprim-Sulfamethoxazole cause in
addition, sulfonamide side
effects--nausea, vomiting,vasculitis,
renal damage.
AIDS patients being treated for
pneumocystis pneumonia have a high
frequency of adverse reactions,
particularly fever, rash, leukopenia
diarrhea.
Chambers, H.F. and Jawetz,
E.Sulfonamides,Trimethoprim, and Quinolones,in Basic and Clinical
Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, p. 761-763.
![]() Adverse effects
Adverse effects
DNA gyrase inhibitors
DNA gyrase inhibitors: The function of DNA gyrases, and the effects of their inhibition; clinical uses of quinolones and fluoroquinolones; adverse effects and potential drug-drug interaction for quinolones.
Drugs to Treat Mycobacterial Infections
Mycobacterial infections are a therapeutic challenge
Slow growth characteristic results in relative resistance to antibiotic therapy. Antibiotic activity is usually directly depend on the rate of cell division
Many mycobacterial organisms are intracellular (residing in macrophages, for example)
Single drug treatment of mycobacterial infections readily promotes development of resistance
Combination therapy over an extended period of time is required for effective treatment.
Mycobacterial infections include those caused by Mycobacterium tuberculosis, M bovis, atypical myocacterial infections, and M. leprae (leprosy)
First line of drugs in order of preference:
Isoniazid (INH)
Rifampin (Rimactane)
Pyrazinamide
Ethambutol
Spectinomycin (Trobicin)
Second Line Drugs
Amikacin (Amikin)
Aminosalicylic Acid
Capreomycin
Ciprofloxacin (Cipro)
Clofazimine
Cycloserine
Ethionamide
Ofloxacin (Floxin)
Rifabutin (Mycobutin)
Mechanisms of Actions of Antimycobacterial Agents
Overview:
Isoniazid (INH) is the most active for treatment of tuberculosis.
INH inhibits mycolic acid synthesis, an essential part of mycobacterial cell walls.
Given alone, INH administration selects out resistant mutants which necessitates additional agents.
At present (1997) about 10% of tuberculosis isolates are INH resistant. INH is well absorbed after oral administration.
Hepatic metabolism by acetylation is influenced by genetic predisposition to fast- or slow acetylation. Dosage adjustments may be required INH metabolites are renally excreted.
Clinical Aspects:
Single-drug use: prevention of active tuberculosis in M. tuberculosis infected individuals who have not developed active disease.
Very young children who are seropositive within two years following a negative skin test and HIV-infected and AIDS patients are candidates for INH preventative treatment.
Single drug: INH treatment is also indicated as a preventative for individuals who have been in close contact with individuals who have active pulmonary tuberculosis.
![]() Adverse
Effects
Adverse
Effects
Fever, skin rash.
Toxicity: INH-induced hepatitis--most frequent major toxic effect (1% incidence, age-dependent with older patients at higher risk and younger patients at much reduced risk).
Peripheral neuropathy which is reduced by pyridoxine supplimentation.
Rifampin (Rimacine)
Overview
Rifampin is a semisynthetic derivative of rifamycin.
Rifampin is active against gram-positive and gram-negative cocci, some enteric organisms, mycobacteria and Chlamydia.
Rifampin binds selectively to bacterial DNA-dependent RNA polymerase thus inhibiting RNA synthesis.
Rifampin is bacteriocidal for myobacteria.
Clinical Uses
Rifampin co-administered with isoniazid or ethambutol to treat myobacterial infections.
Rifampin in combination with a sulfone (dapsone) is used to treat leprosy.
Rifampin is a substitute for INH tuberculosis prophylaxis.
Other Uses: Prophylaxis for Haemophilus influenzae type children contact
Rifampin with another agent to eradicate staphylococci
Combination therapy for serious staphylococcal infections including osteomyelitis and prosthetic valve endocarditis.
Rifampin in combination with ceftriaxone or vancomycin to treat meningitis caused by highly penicillin-resistant pneumococcal isolates
![]() Adverse
Effects
Adverse
Effects
Harmless orange coloration to urine, sweat, tears.
Occasional effects: rash, nephritis, thrombocytopenia, flu-like symptoms depending on dosing intervals
Rifampin microsomal P450 induction increases the metabolism of many drugs
Chambers, H.F. and Jawetz, E.Antimycobacterical Drugs ,in Basic and Clinical Pharmacology,(Katzung, B. G., ed) Appleton-Lange, 1998, pp. 770 - 773