Coronary Artery Disease and Anesthesia Management
Regulation of coronary blood flow
Normal physiologic regulation:
Autoregulation in response to myocardial metabolic requirements
Coronary flow increases with metabolic demand
Abnormal physiological regulation in the presence of atherosclerotic coronary vessel disease
Atherosclerosis:
Physical obstruction of the coronary vasculature
Impairment of autoregulation
Consequences of an increase in myocardial oxygen demandspace for (or reduced myocardial oxygen supply) in the presence of atherosclerotic coronary vessel disease
Myocardial ischemia
Major intraoperative goal for anesthesia providers:
Prevention/treatment of intraoperative cardiac ischemia -- method:
Minimize cardiac O2 demand
Maximize cardiac O2 supply
Myocardial Oxygen Demand: Major Determinants:
Myocardial wall tension
Cardiac contractility state
Intraoperative prevention of excessive myocardial O2 demand:
Before coronary revascularization, positive inotropic agents should be avoided (since the increase contractility thereby increasing O2 demand)
Excessive myocardial contractility may be reduced by anesthetics, which act by limiting sympathetic stimulation
With adequate cardiac function ß-adrenoceptor blocking agents may be used to diminish contractility
Anemia increases myocardial O2 demand while concurrently reducing myocardial O2 supply
Intervention: consider pre-bypass transfusion (given the transfusion will be required during bypass or post-bypass time frame)
Therapeutic intervention: Balancing myocardial O2 supply and O2 demand requirements--
Example #1: ß-adrenoceptor blockade-- use of ß-blockers (e.g., propranolol (Inderal); metoprolol (Lopressor))
Reduces cardiac O2 demand by attenuating contractility (negative inotropism) increases mediated by increased circulating catecholamines levels and sympathetic nervous system activity
Reduced heart rate (negative chronotropism) increases diastolic filling time, thereby increasing time available for coronary vascular perfusion
Example #2: Blood pressure reduction
Advantage: reduced myocardial oxygen consumption (reduced afterload)
Disadvantage: reduced coronary blood flow through stenotic regions
Overall objective -- both limitation in myocardial oxygen demand and maximization of supply: anesthetic should optimize this balance
Myocardial Oxygen Supply: Major Influences:
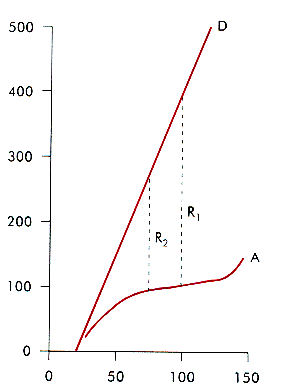
Autoregulation: Constant flow despite significant blood-pressure variations
Anemia: blood flow increases to ensure adequate O2 delivery to the myocardium
With maximal vasodilation, coronary blood flow is related linearly to blood pressure-- Definition "coronary vascular reserve" = blood flow beyond that which would normally occur with intact autoregulation.
 |
|
Diastole: Importance in maintaining adequate myocardial oxygen supply
Reason: a significant percentage of epicardial and nearly all middle cardial and endocardial coronary flow occurs during diastole--this principle applies primarily to the left ventricle since significant right ventricular coronary flow occurs during systole
Consequence: diastole defines the time available for coronary blood flow
Tachycardia: detrimental secondary to diastolic interval reduction; ¯ ¯ reduced flow
Implication: significant coronary flow may be accomplished by reducing/avoiding conditions producing tachycardia (bradycardia however, is probably not desirable in terms of increasing epicardial coronary flow)
Diastolic Ventricular Filling Pressure-- a factor that opposes coronary blood flow
Blood flow through the myocardium is based on a pressure differential between (a) proximal coronary driving pressure and (b) distal opposing pressure
Definition:
proximal coronary driving pressure = considered to be the aortic pressure throughout diastole (note that the aortic pressure will be decreasing during diastole, therefore the driving force will not be constant)
Distal opposing pressure: measurement suggestions have included the ventricular wall pressure or LVEDP (left ventricular end diastolic pressure) or coronary sinus pressure
For clinical applications: LVEDP is used because it may be readily estimated and it is related directly to the myocardial region most susceptible to ischemia, the subendocardium
The actual driving pressure therefore is not the aortic diastolic pressure but rather whatever residual pressure is present, distal to stenotic region
In patients with coronary vascular disease, the pressure gradient which drives coronary blood flow may be small in influence significantly by LVEDP (wedge pressure)
Clinical consequence: anesthesia providers must carefully monitor ventricular filling pressures using the pulmonary artery catheter
Nitroglycerin may be used to maintain optimal filling pressures
Optimization of coronary perfusion pressure gradients involved typically:
Raising the diastolic arterial pressure
Decreasing LVEDP (left ventricular and diastolic pressure)
Special Clinical Considerations
Patient exhibits both elevated filling pressures and hypotension
Question: Can nitroglycerin be administered safely/appropriately?
Answer: Yes, however the arterial pressure must be protected
Judgment Issues with respect to myocardial contractility
Left ventricular function is very poor: use epinephrine or norepinephrine (Levophed) \to provide inotropic support before nitroglycerin is administered
Left ventricular function is satisfactory: increase arterial pressure using a pure vasoconstrictor, then add nitroglycerin
Avoid: Do not add fluids -- BP will probably remain unchanged but increased filling pressure is likely to worsen coronary blood flow, particularly to the left ventricular subendocardium
Concern: nitroglycerin reduces preloaded come the causing the decrease in cardiac output
Response: The primary objective is to improve/increase coronary blood flow, not cardiac output
Interventions which both decrease filling pressures (vasodilators, e.g. nitroglycerin) and increase BP (a-adrenergic receptor agonists) may increase cardiac output, secondary to reduced myocardial ischemia
Other ways of improving myocardial O2 delivery:
Increased inspired O2 concentration
Correction of preoperative anemia
Anesthetic protocol should:
Improve/facilitate myocardial oxygen delivery
Block sympathetic responses that would tend to increase myocardial oxygen requirements
Primary goal: Enhance oxygen delivered to the heart (not to increase cardiac output)
Administering fluids to increase cardiac output is likely inappropriate as long as sufficient systemic perfusion avoids metabolic acidosis [increase filling pressures may readily degraded coronary perfusion pressure gradients]
Positive inotropic drugs should not be used unless needed to increase contractility sense these agents increase myocardial oxygen demand and thus might promote an ischemic state
| Hemodynamic event | Pharmacological intervention |
|
|
|
|
|
|
|
|
|
|
|
|