|
|
|
1Mechanisms involved in pathology associated with
asthma
A generalized tracheobronchial hyperirritability is a central
aspect of asthma. Airway reactivity may vary and with heightened reactivity more
obvious and severe symptoms present and more aggressive
pharmacotherapy are required. Lung function exhibits
fluctuations throughout the day with dyspnea more apparent at
night and in the early morning. Airway reactivity varies in all individuals as a function of
exposure to oxidant air pollutants as well as following
respiratory tract viral infections. Of these two insults, viral
infections are more predominant in their long-term effects on
airway reactivity. Furthermore, allergens produce rapid
increases in airway responsiveness (reactivity) which remains
heightened for weeks. With significant allergen exposure,
obstruction may occur rapidly and last for some time. The current working framework for the understanding of
asthma is based on the presence of continual airway inflammation
which can be exacerbated under certain circumstances.
Asymptomatic asthmatic patients therefore exhibit the
presence of inflammation confirmed by endobronchial biopsy.
The airway is characterized as edematous with eosinophil,
neutrophils, and lymphocyte infiltration. Increased
capillary density with increased cellularity represents
probably the most common finding. Overall asthma manifestation is probably a complex result
of interactions between airway inflammatory cells,
inflammatory mediators, cytokines, and surface epithelium.
Cell types most likely involved include mast cells,
eosinophils, epithelial cells, and lymphocytes. Also, there
is the possibility of macrophage and neutrophil involvement.
Cells primarily involved release mediators which include:
histamine, leukotrienes (C, D
and E), bradykinin,
platelet-activating factor, and prostaglandins (E2,
F2 Bradykinin Histamine (as the chloride)
Prostaglandin F2 Prostaglandin
D2
Arachidonic Acid Pathway (Leukotriene,
Prostaglandin, Thromboxane Synthesis
Leukotriene C4
Leukotriene D4
Leukotriene E4
Leukotriene B4
Platelet Activating Factor,
1-alkyl, 2-acetyl phosphatidylcholine
The above mediators produce an immediate, intense
inflammation that is characterized by vascular congestion, edema,
and bronchoconstriction. Leukotrienes which act to promote airway smooth
muscle contraction as well as mucosal edema also may inhibit
mucociliary transport and increase mucus production. Chronic events follow these initial actions with
chemotactic factors recruiting eosinophils, polymorphonuclear
leukocytes, and platelets to the reaction site. ("Chemokines:
(chemoattractant cytokines) are short soluble peptides (70-90
amino acids) which can be divided into two groups. Alpha
(or C-X-C) chemokines contain a single amino acid between the first
and second cysteine residues, and are primarily involved in
neutrophil activation. Beta (or C-C) chemokines have adjacent
cysteine residues and are generally involved in activation of
monocytes, lymphocytes, basophils and eosinophils"6).
These chemotactic factors include eosinophil and
neutrophil anaphylactic factors and leukotriene B4. These
recruited cells in addition to macrophages already present as well
as the bronchial epithelium provides sources for additional
mediators enhancing immediate and cellular phases.
Airway epithelial cells serve both as a
target and a contributor to the inflammation process since they
amplifying the bronchoconstrictive aspect by liberating endothelin-1
and enhance vasodilatation by liberation of nitric oxide (
![]() ,
and D2).
,
and D2).
![]()


![]() ), PGE2 as
well as the 15-hydroxyeicosatetranoid acid (15-HETE)
arachidonic acid metabolic products.
These cells also produce cytokines including:
), PGE2 as
well as the 15-hydroxyeicosatetranoid acid (15-HETE)
arachidonic acid metabolic products.
These cells also produce cytokines including:
Eotaxin is an eosinophilic chemoattractant cytokine which is upregulated in allergic airways inflammation. Figure below: attribution--Tim Williams PhD, Imperial College of Medicine, South Kensington, London
8The accumulation of eosinophilic leukocytes in the lungs of asthmatic patients is probably due to the effect of chemoattractant small molecules. Eotaxin has been identified as a potent eosinophil chemoattractants that is produced by several different cells in the stimulated by interleukin-4 and interleukin-13, both of which are synthesized by T-helper (Th)2 lymphocytes.
8Eotaxin interacts with the eotaxin receptor which is a C-C chemokine receptor (CCR)3. Small molecules have been synthesized without interfere with eotaxin binding to its chemokine receptor, suggesting a possible therapeutic intervention that will limit eosinophilic recruitment in the lung with subsequent possible prevention of damage and pulmonary dysfunction.
8The eosinophil represents a white cell that has a two-lobed (bilobed) nucleus and has cytoplasmic granules which stain pink following exposure to eosin.
It has been suggested that eosinophils are important in the immunological defense system against helminths (worms).
Parasitic worms causing immunological response particularly towards TH2 lymphocytes which regulate IgE production. Immunoglobulin E binds to mast cells providing the means for specific antigen recognition (especially important in acute responses to worms).
TH2 lymphocytes regulate eosinophil accumulation important chronic responses to worms.
In eosinophils accumulating around these parasites then become stimulated to release O (free radicals) molecules as well as toxic proteins including basic protein, eosinophil peroxidase, eosinophil cationic protein and eosinophil-derived neurotoxin.
According to this view, allergy may be a host response originally developed against helminths but now triggered in an inappropriate manner by other stimuli.
The particular importance of eotaxin is that it provides the mechanisms by which selective eosinophil accumulation may be mediated, given that other chemoattractants have more generalized effects (i.e. they promote neutrophil attraction; these other chemoattractants include C5a, leukotriene B4 and platelet-activating factor)
8Concerning the eotaxin receptor: there been > 50 chemokines identified which mediate effects through at least 15 different 7-transmembrane-spanning, G-proteins-coupled receptors.
Most chemokines produce effects by mediation through several different receptors; however, eotaxins are fairly unusual in that there signaling process involves a single receptor, the CCR3 receptor which has been cloned and noted to be highly expressed on eosinophils.
The CCR3 receptor has been found also on TH2 lymphocytes which regulate eosinophilic recruitment.
Following eotaxin binding with theCCR3 eosinophil surface receptor a number of molecular events occur in including: calcium mobilization, CD11b up-regulation, mitogen-activated protein kinase activation, oxygen radical production, actin polymerization and receptor confomrational change which is connected to granule release and chemotaxis. Mechanisms for CCR3 internalization have also been described.
|
|
|
|
|
|
|
|
1 Whereas the mast cell is important in the early stages of the reaction, eosinophils play a central role in the infiltrative aspect.
Granular eosinophilic proteins (eosinophilic cationic protein and basic protein) as well as oxygen-derived free radicals probably destroyed the airway epithelial lining medicine and sloughed into the bronchial lumen as 5Creola bodies.
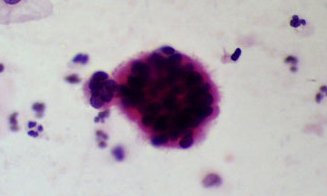
5Attribution for the Creola body image: S U N Y Upstate Medical University, Content maintained by: Susan Stowell, copyright © 2002, SUNY Upstate Medical
5"Creola bodies ...are characterized... by cilia, the evenly distributed chromatin, and the smooth nuclear membranes"
1 Damage described above not only affects barrier and secretory processes but also causes additional chemotactic cytokine production which promotes additional inflammatory responses. Such localized processes may translate to generalized reactions secondary to activation of neurogenic inflammatory pathways possibly by direct excitation of sensory nerve endings.
T lymphocytes are central to the inflammatory response with an increased presence in the asthmatic airway; furthermore,T lymphocytes are activators of cell-mediated immunity through cytokines as well as humoral (IGE) immune reactions.
T- activated lymphocytes which
have been harvested from asthmatic patient lungs express mRNA
for those cytokines involved in eosinophil and mast cell
recruitment + activation. With respect to subpopulations,TH1
andTH2 lymphocytes both probably influence asthma
responses. For example, cytokines IL2 and interferon (IFN) ![]() , Substances Produced by TH1 Lymphocytes promote
differentiation and growth of Type B lymphocytes and cause
macrophage activation, Respectively. Similarly IL-4 and
IL-5, TH2 cytokine products promote B-cell growth
and immunoglobulin secretion [IL-4] and eosinophil
proliferation, differentiation, and activation [IL-5].
, Substances Produced by TH1 Lymphocytes promote
differentiation and growth of Type B lymphocytes and cause
macrophage activation, Respectively. Similarly IL-4 and
IL-5, TH2 cytokine products promote B-cell growth
and immunoglobulin secretion [IL-4] and eosinophil
proliferation, differentiation, and activation [IL-5].
1 Cytokine production:
This process is an important, vital component in asthma inflammatory processes. Cytokines synthesized and released from these inflammatory cells discussed earlier as well as from epithelial cells, fibroblasts, endothelial cells, and airway smooth muscle activate many specific cell-surface receptors.
Cytokines that are thought to most important in asthma pathogenesis and are secreted by T lymphocytes are:
IL-3 -- lengthens mast cell surviva
IL-4 and IL-13 -- activates B lymphocytes IgE synthesis and adhesion molecule expression.
IL-5 -- differentiation and lengthens eosinophil survival.
Pro- inflammatory cytokines
which also could amplify the inflammatory response include
IL-1B, IL-6, IL-11, tumor necrosis factor ![]() (TNF-
(TNF-![]() )
and GM-CSF
.
)
and GM-CSF
.
|
|
Asthma: Systems Pathophysiology
Pathophysiologic Manifestations:
Airway diameter reduction, caused by smooth muscle contraction, vascular congestion, bronchial wall edema and thick, tenacious secretion.
Consequences of Airway Diameter Reduction in Acute Asthma
increased airway resistance
decreased forced expiratory rates
increased work of breathing
changes in respiratory muscle function
changes in elastic recoil
abnormal ventilation/pulmonary blood flow distribution
ventilation/perfusion mismatching
lung and thorax hyperinflation

image from: ©Edward C. Klatt MD, Department of Pathology, University of Utah, Salt Lake City, Utah, USA, and by designated contributors: used with permission; http://www-medlib.med.utah.edu/WebPath/webpath.html#MENU
9Compromised pulmonary function in Asthma:
ECG changes indicative of right ventricular hypertrophy and pulmonary hypertension
vital capacity < 50% of normal
1 - second forced expiratory volume (FEV1): reduced to 30% of expected
maximum/a minimum midexpiratory flow rates: reduced to 20% or less of expected
in acute illness: residual volume (RV): may approach 400% of normal; functional residual capacity doubles
patients report that the attack has ended clinically when RV has fallen to 200% of expected and FEV1 reaches 50% of expected level
very common finding during acute phase
respiratory failure -- relatively uncommon: 10% to 15% of presenting patients
hypercapnea: common
respiratory alkalosis: common
Normal arterial carbon dioxide tension but severe airway obstruction present is suggestive of possibly impending respiratory failure
Metabolic acidosis in acute asthma with severe obstruction
Clinical presentations may not correlate with blood gas data; however, estimating patient's ventilatory state solely on clinical presentation may be dangerous
Patients with possible alveolarhypoventilation should have arterial blood gas tension measurements
Cyanosis: -- very late sign; suggestive that extreme hypoxia may go undetected.
Some Clinical Features in Asthma:
There are three principal symptoms that characterize asthma. These are dyspnea, cough, and wheezing with wheezing being particularly prominent.
As we have noted earlier, asthma is an episodic disorder with the above symptoms commonly exhibited.
Initially patients experienced chest constriction perhaps with a nonproductive cough.
Audibly harsh, wheezing respiration is then noted; expiration is prolonged and difficult.
Tachypnea, mild systolic hypertension and tachycardia are frequent presentations.
Lung overinflation is typical in the anterioposterior thoracic dimension (diameter) increases.
Severe or prolonged asthma attacks are associated with a loss of adventitial breath sounds along with notably high pitched wheezing.
Respiratory accessory muscles become more prominent as well as paradoxical pulse-signs indicative of severe obstruction with impaired, significantly impaired pulmonary function.
Paradoxical pulse requires significantly large negative intrathoracic pressures; therefore, with shallow breathing, condition which does not favor development of large negative intrathoracic pressures, significant obstruction can be present even in the absence of paradoxical pulse.
[Paradoxical pulse definition: Inspiratory decrease in arterial pressure >10 mm Hg with Inspiratory venous pressure unchanged (Kussmaul's Sign); Paradoxical pulse signs: Palpable decrease in pulse with inspiration Inspiratory systolic blood pressure decreased over 10 mm Hg less than expiratory pressure]. Significant disease may remain if the endpoints are only an a reduction in wheezing and the resolution of subjective complaints.
The conclusion of an asthmatic episode may be associated with coughs producing a thick, stringy me at this in the form of distal airway casts (Curschmann's spirals) which when microscopically evaluated shows the presence of eosinophils and Charcot-Leyden crystals.
Severe mucus plugging with possibly imminent suffocation may occur and in this case the cough would be ineffective and the patient will be gasping. Such circumstances may necessitate mechanical ventilation. Atelectasis (collapsed lung) may also occur in asthma.
"CHARCOT LEYDEN CRYSTALS, MICRO - Eosinophilic needle-shaped crystalline structures. Represents breakdown products of eosinophils. Seen in asthma and eosinophilic pneumonia."
Bronchial wall characteristics during an acute asthma attack:
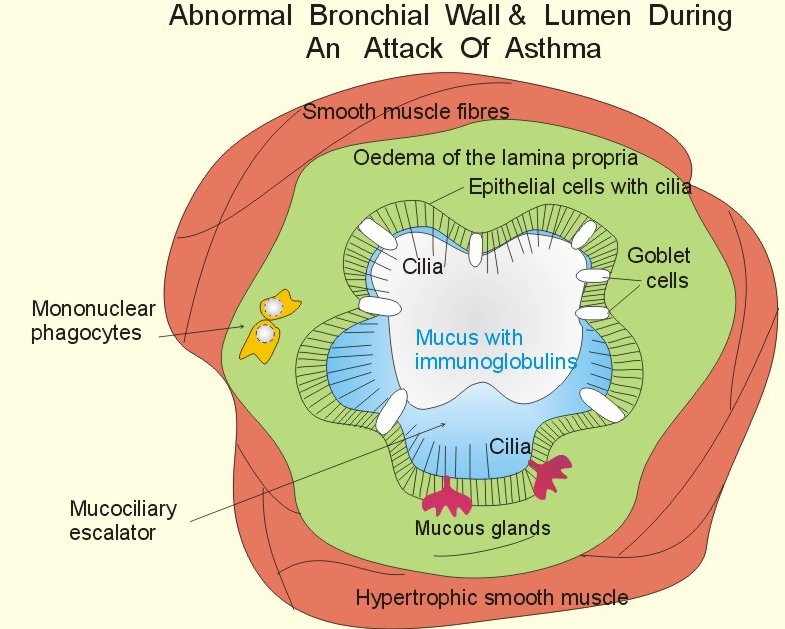
Above Figure from: Chapter 13 in: Textbook in Medical Physiology And Pathophysiology Essentials and clinical problems Copenhagen Medical Publishers 1999 - 2000, Poul-Erik Paulev, M.D., D.Sci (http://www.mfi.ku.dk/ppaulev/chapter13/Chapter13.htm), used with author's permission
Animation of asthmatic breathing cycle noting residual lung volume (copyright (C) 1996, Stephen M. Borowitz)

1 McFadden, E.R., Jr. "Asthma: Diseases of the Respiratory System" in Harrison's Principles of Internal Medicine, 15th Edition (Braunwald, E., Fauci, A.S., Kasper, D.L., Hauser, S.L, Longo, D.L. and Jameson, J. Larry, eds) pp. 1456-1463, McGraw-Hill Medical Pubishing, Division, New York, 2001
2 Kelley, H. William, "Asthma" in Pharmacotherapy: A Pathophysiologic Approach, (Dipiro, J.T., Talkbert, R.L. Yee, G.C., Matze, G.R., Wells, B.G. and Posey, L. Michael, eds.) pp 430-459. McGraw-Hill Medical Pubishing, Division, New York, 1999.
3Spencer SM., Sgro JY., Dryden KA., Baker TS., Nibert ML. (1997) Rhinovirus 14 (3D image reconstruction from electron microscopy data) Journal of Structural Biology. 120(1):11-21
4Attribution: Michigan State University
5State University of New York, Upstate Medical University, Cytotechnology, On-Line Courseware
6Steve Dewhurst, Ph.D., Structure of the CC-chemokine, RANTES, (c) University of Rochester and Stephen Dewhurst, 1999
7Ealick SE, Recombinant Human Granulocyte-Macrophage Colony-Stimulating Factor, Cornell University, http://arginine.chem.cornell.edu/Structures/GMCSF.html
Walter MR, Cook WJ, Ealick SE, Nagabhushan, TL, Trotta, PP and Bugg, CE. Three-Dimensional Structure of Recombinant Human Granulocyte-Macrophage Colony-Stimulating Factor, J. Mol. Biol. 224:1075-1085 (1992).
Reichert P, Ealick SE, Cook WJ, Trotta P, Nagabhushan TL, Bugg CE. Crystallization and Preliminary X-ray Investigation of Human Granulocyte-Macrophage Colony Stimulating Factor, J. Biol. Chem. 265(1):452-453 (1990)
8Williams, TJ and Conroy, TM Eotaxin and the attraction of eosinophils to the asthmatic lung, Respir Res 2001, 2: 150-156
9McFadden, Jr., E. R., Diseases of the Respiratory System: Asthma, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, p 1422.
10Daroca, P, Lung and Respiratory System
Review, Tulane University Pathology, (Figure and caption
attribution)