|
|
|
Anesthesia Pharmacology Chapter 19: Co-Existing Conditions (Asthma)
|
|
1 Asthma is most correctly defined as a chronic inflammatory airway disease associated with excessive tracheobronchial reactivity.
The reactive airway may be provoked by a number of stimuli. Airway constriction may resolve following pharmacological intervention or spontaneously; however, manifestations including wheezing, cough, and dyspnea are prevalent.
Before considering implications of asthma and other pulmonary disease in the context of preoperative, and properties, and postoperative anesthesia management, we shall consider basic physiological, pathophysiological, and biochemical aspects of pulmonary disease generally.
"Asthma is a chronic inflammatory disorder of the airway is, in which many cells and cellular elements play a role, in particular, mast cells, eosinophils, T-lymphocytes, macrophages, neutrophils, and epithelial cells. In susceptible individuals, this inflammation causes recurrent episodes of wheezing, restlessness, chest tightness, and coughing, particularly at night or early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli."--Expert Panel of the National Institutes of Health, National Asthma Education and Prevention Program (NAEPP)
By way of background, asthma is characterized by relatively asymptomatic periods with occasional acute attacks.
These episodes may resolve fairly rapidly pursuant to pharmacological intervention; moreover, sometimes patients may chronically experienced some degree of airway resistance. A serious condition, status asthmaticus, occurs when significant obstruction persists for extended periods. Status asthmaticus is defined as a therapeutic emergency.
Asthma affects about 5% of the United States population, which corresponds to about 14-15 million individuals in the United States.
This frequency is comparable to that observed in other countries. Typically asthma is first noted early in life, although it occurs at all ages.
In terms of age distribution about 50% of cases are noted in patients less than 10 years of age with another 33% occurring before the age of 40. Initially (childhood), males appear about twice as likely to present with asthma as females; however, this the gender difference is not noted following the age of 30.
Asthma, affecting about 5 million children, is the most common chronic illness among children with minorities particularly affected. African-American individuals exhibit about 19% higher asthma incidence compared to whites and are two times more likely to be hospitalized for asthma.
Based on 1990 data, about 10 million schooldays were missed due to asthma resulting in a cost of about $1 billion due to lost family income.
Another concern is the trend indicated in the timeframe from 1980-1993 that the "age-specific" death rate due to asthma increased file over twofold.
Asthma mortality appears highest among African-American individuals indicated by a 400% higher likelihood of death compared to other groups.
From the point acute classification, one approach has been to categorize based on the factor(s) that precipitate the occurrence, although this approach may be overly simplistic given the heterogeneous nature of asthma.
Generally, following this approach, "allergic" and "idiosyncratic" are the two principal types of asthma classifications.
1Atopy ("hereditary allergy characterized by symptoms [as asthma, hayfever, or hives] produced upon exposure to the exciting antigen without inoculation" Merriam-Webster Collegiate dictionary) constitutes the largest risk factor for asthma development.
1Allergic asthma is associated with a family history (or personal history) of allergic diseases including urticaria (hives), rhinitis, and/or eczema with positive wheal-and-flare reactions to intradermal injection of airborne antigen extracts and would be associated with increased levels of serum IGE and/or positive response to specific inhaled antigen.

1Many individuals do not exhibit personal/family allergy history and shell normal IGE serum levels and negative skin tests.
Consequently, this type of asthma is not classified within immunological context and is instead described as idiosyncratic asthma. In this setting the initial provocative event for asthma development may be an upper respiratory illness.
In particular, the initial event could be a common cold but wheezing and dyspnea which may last four days-months may be exhibited within a few days.
This phenomenon is different from an individual with chronic bronchitis or bronchiectasis and could then manifest bronchospasm as a consequence.
Factors that may trigger an asthmatic reaction
"Human infant lung, post-mortem tissue: immunohistochemical staining for Respiratory syncytial virus (RSV) using NCL-RSV3. Note intense staining of infected luminal bronchial epithelial cells. Paraffin section." Image: © 2002 Novocastra Laboratories Ltd (http://www.novocastra.co.uk/mvph.htm). |
|
|
|
|
|
|
|
|
Cold Air
Fog
Wood smoke; tobacco smoke
Ozone
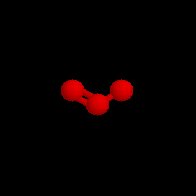
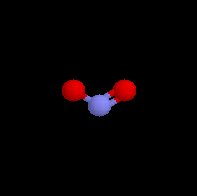
Nitrogen dioxide

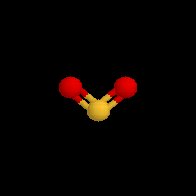
Sulfur dioxide
![]()
|
|
Stress
Laughter
Anxiety
Exercise (dry, cold weather especially)
2Drugs and Agents used as Preservatives
Aspirin
Nonsteroidal anti-inflammatory agents (NSAIDS) COX; COX-2 inhibitors (e.g. Valdecoxib (Bextra))--
Arthrotec (diclofenac/ misoprostol), celecoxib (Celebrex),diclofenac (Voltaren, Cataflam),diflunisal (Dolobid),etodolac (Lodine), flurbiprofen (Ansaid), Ibuprofen (Motrin), Indomethacin, ketoprofen (Orudis), ketorolac (Toradol), nabumetone (Relafen), naproxen (Naprosyn), piroxicam (Feldene), rofecoxib (Vioxx), salsalate (Disalcid), sulindac (Clinoril)
Sulfites (preservative)
Benzalkonium chloride (preservative/detergent)
![]() -adrenergic
receptor antagonists, e.g. propranolol, metoprolol, atenolol,
timolol
-adrenergic
receptor antagonists, e.g. propranolol, metoprolol, atenolol,
timolol
Propranolol (Inderal), 
Agents encountered in the work place
Flour dust (Bakers)
Hay mold (Farmers)
Formaldehyde, western cedar, dimethylethanolamine, anhydrides (Plastics, rubber and wood workers)
Arabic gum (Printers)
Azo dyes, anthraquinones, ethylenediamine, toluene diisocyantes, polyvinyl chloride (Chemical workers)
Allergic asthma require is an IGE response.
The IGE response is determined by T- and B lymphocytes. Central to the processes is the interaction of antigen with mast cell-bound IgE molecules. Anatomically, airway epithelium and submucosa include dendritic cells which process antigen.
Dendritic cells, following uptake of antigen, move to local lymph nodes, there presenting material to T-cell receptors.
In some circumstances (perhaps genetically determined) antigen interaction with naive T cells (TH0) in the presence of IL-4 results in TH0 cell differentiation to a TH2 cells.
Concurrently, this process, while facilitating asthma inflammation, also promotes B lymphocyte transformation from IgG and IgM production to IgE production.
Following sensitization due to prolonged antigen exposure, very small amounts of antigen can produce significant worsening of the chronic underlying disease (asthma).
The central role of immune processes is reflected in the causal relationship in asthma in about 33% of all cases with contributory involvement in probably another 33% of cases.
Although allergic asthma is typically seasonal, nonseasonal asthma can result from continued exposure to animal danders, dust mites, molds, etc.
Antigen exposure can induce an immediate airway obstruction response within the minutes timeframe with fairly rapid resolution. However, in 30%-50% of cases, a late reaction which is another bronchoconstrictive event, may occur from 5-10 hours later. Sometimes only this late reaction is observed.
The initial response to inhale allergen probably depends on antigen-Ab interactions on pulmonary mast cells with subsequent rapid release of mediators.
|
|
1 Drugs as stimulatory with respect to the Asthmatic Response
1 Acute asthma attacks may be induced by certain drugs, the most common of which include beta-adrenergic antagonists, sulfite-containing agents, aspirin, and coloring agents such as tartrazine.
Significant morbidity is associated with drug-induced bronchial constriction with death having been attributed to aspirin (or other nonsteroidal anti-inflammatory drugs) or beta adrenergic blocker ingestion.
Aspirin-induced asthma appears to occur more frequently in adults relative to children. In aspirin sensitivity may begin with a vasomotor rhinitis (perennial) which leads to nasal polyps (hyperplastic rhinosinusitis).
|
|
|
Asthma exacerbation may be induced by elevated concentrations of atmospheric pollutants/antigen's which may occur in particularly industrial or densely populated cities.
Such accumulation is favored under certain weather conditions which create relatively stagnant air (thermal inversions).
Asthmatic patients will be most severely affected, although the general population will also perceive respiratory effects.
Ozone, nitrogen dioxide and sulfur dioxide have been identified as particularly important air pollutants in this regard, although sulfur dioxide requires both a high ventilatory rate and concentration.
Airborne antigens (pollen) can seasonally rise to sufficient concentrations to markedly increased hospital admissions as well as death rates. Seasonal effects may be diminished impact by early use of anti-inflammatory agents.
Prolonged exposure in the workplace to a variety of substances may exacerbate asthma or induce an asthma attack.
Bronchoconstriction may occur as a result of exposure to metal salts such as platinum, nickel or chrome.
Other concerns involves wood or vegetable dust, certain drugs such as antibiotics, cimetidine, as well as industrial chemicals and plastics.
Enzymes found in detergents and animal/insect dusts, serums, or secretions may also be provocative substances.
These chemicals may also be found outside the workplace environment.
This type of airway obstruction appears to involve three possible underlying mechanisms:
(1) the agent induces the formation of a specific IgE (resulting in an immediate, late, or dual immunological reaction)
(2) the agent reflexively or directly causes airway stimulation in the asthmatic patient
(3) the agent directly causes bronchoconstrictor substance liberation.
Acute worsening of asthma would be most likely due to respiratory infection.
The major factor is not bacterial or allergic responses to microorganisms would rather is a respiratory virus.
In children the two most important viruses would be respiratory syncytial virus and parainfluenza virus. In the older child in adults, rhinovirus and influenza virus would be more common.
An active respiratory tract infection is necessary to induce the asthma attack, going beyond colonization. In the individual whose asthma had been under control, such a respiratory infection can destabilize the condition for extended periods, e.g. weeks.
A possible basis for this effect would be a viral-induced production of T-cell-derived cytokines which promote inflammatory cell infiltration into the airway.
Acute asthma attacks are often provoked by exercise.
Exercise, differing from other provocative factors, is not produce long-term effects and does not increase intrinsic airway reactivity.
Bronchospasm can be induced by exercise in essentially every asthmatic patient and in some cases it is the only provocative act (at least initially) or exposure that causes asthmatic symptoms.
The severity of exercise-induced bronchoconstriction include ventilatory levels as well as humidity and temperature of the inspired air.
The direction of the effect is that higher ventilation rates with reduced air temperature tend to promote greater obstructive responses.
Running as opposed to walking causes a more severe asthmatic attack, even if the air temperature + humidity are the same in both cases.
Furthermore for any given exertional task, cold air will tend to enhance the obstructive response and warm, humid air would likely reverse the effect.
With respect to specific sports then, ice hockey and cross-country skiing our activities that would be more likely to cause an asthma attack then swimming inside, in a heated pool.
A possibility, in terms of mechanism that might explain exercise-induced obstruction, involves thermal induction of hyperemia with microvascular engorgement of the bronchial wall.
Psychological factors appear to interact with underlying asthma pathophysiology either to worsen or improve the disease state.
The psychological effects appear important to about 50 percent of patients.
Physiologically, airway caliber may be modulated through vagal efferent activity although endorphins may also contribute.
Patients may be "suggestible" with suggestion resulting in changes in adrenergic and cholinergic stimuli effects on airway.
Psychophysiological effects appear variable from patient to patient and possibly variable within a patient depending on the nature of the episode.