|
Adverse Systems physiological
Effects of postoperative pain
Pulmonary system (decrease lung volumes
secondary to patient's pain associated with respiration)
|
Pneumonia |
Hypercarbia |
Atelectasis*
(total/partial collapse
of the lung) |
ventilation/perfusion
mismatching |
arterial hypoxemia |
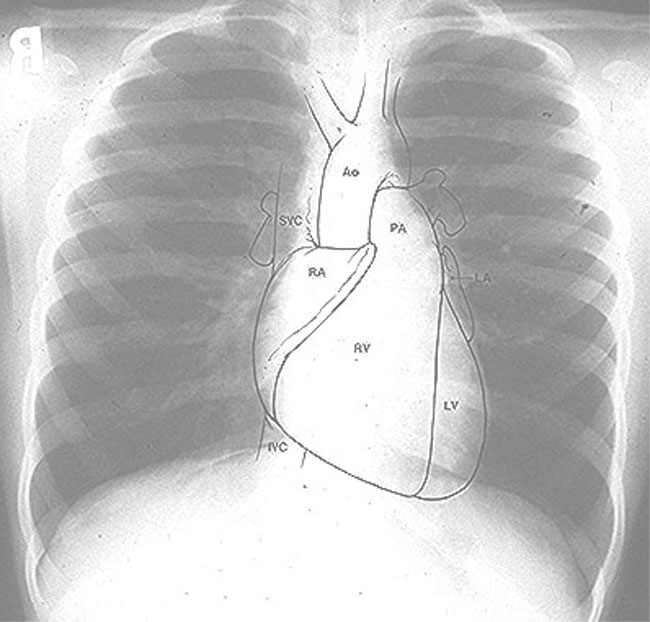
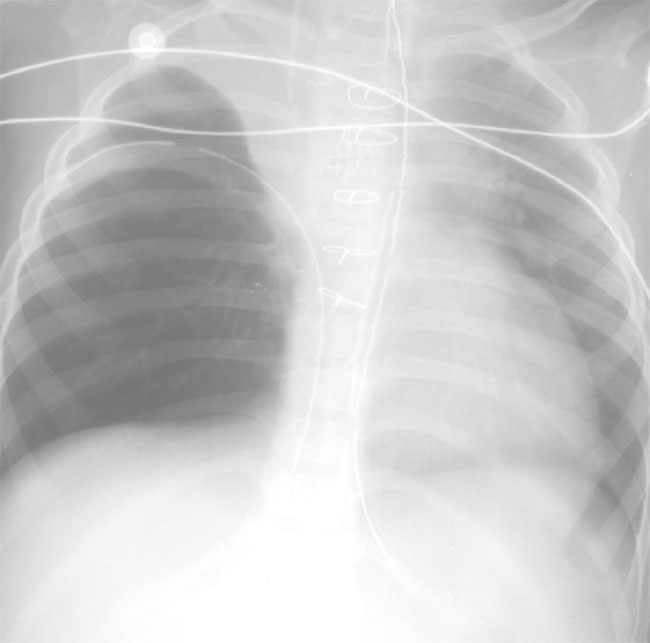
Normal Chest Radiograph (A, left) and one
illustrating Post-operative Atelectasis (B, right)
|
|
|
-
(B, above) Post-operative atelectasis may
occur following surgical correction of congenital heart disease.
-
Texas Children's Hospital, Houston, Texas; Texas Heart Institute; Edward B. Singleton Diagnostic Imaging Service;Colin McMahon,
M.B.BCh. Edward Singleton, M.D.
Atelectasis-Right Middle Lobe
|
Atelectasis-Right Middle Lobe
-
Atelectasis is the loss of lung volume and therefore a direct sign is the displacement of interlobular
fissures. Generally this is accompanied by increased density and possibly elevation of the
hemidiaphragm, mediastinal displacement, or compensatory over-inflation. If there has been
resorption of air within the atelectatic segment, there is generally an absence of air
bronchograms. The pattern of the specific lobar or segmental collapse
produces relatively specific findings on the chest film, often requiring both PA and lateral films for clear and
specific definition.
-
PA (posterior-anterior) radiograph of this female patient (note breast shadows bilaterally) showed
obscuration of the lower right cardiac border merging with opacification of the lung field underlying the right
breast. Because the right middle lobe is immediately adjacent to the cardiac silhouette in that position
collapse or opacification of the right middle lobe will merge densities between the lung and the heart and
thus, the normal sharp boundary between heart and lung is
lost."
-
Yale University School of Medicine, used with permission
|
Medical Editor
C. Carl Jaffe, MD, FACC
Professor of Medicine
(Cardiology)
Section of
Cardiovascular Medicine |
Site producer
Patrick J. Lynch, MS
Design Director
Web Design and Development
Information Technology
Services - Medicine |
|
|
-
Example: thorax/abdominal surgical procedures: question: in this
setting is how would pain lead to respiratory complications:
-
Pain causes in increase in skeletal muscle tension which in
turn reduces total lung compliance, causes hypoventilation and
splinting (splinting is defined as "rigidity of muscles
occurring as a means of avoiding pain caused by movement of the
part" ). These changes cause subsequent effects
including:
-
Additional ventilation/perfusion anomalies (some anomalies
may occur is a result of increases in extracellular lung
water) which promotes hypoxemia
-
This effect reduces significantly functional
reserve capacity [25%-50% of preoperative levels]
-
Pain through its hypoxemia effect results tachypnea &
hypocapnia initially; however, this increase in breathing
work can result in hypercapnic respiratory failure
-
Hypoventilation, induced by pain, can promote pulmonary
consolidation/pneumonitis which at the very least complicates
clinical situation. The significance of these adverse
effects may ultimately depend on the clinical condition of the
patient, e.g. presence of pre-existing pulmonary dysfunction,
advance age, obesity, as well as the particular surgical procedure.
Possible Cardiovascular System Effects
(secondary to excess sympathetic* outflow due to acute
postoperative pain)
|
tachycardia |
systemic
hypertension |
ischemia |
arrhythmias |
-
2*-Increased sympathetic outflow
secondary to painful stimulation can itself enhance, that is
increase pain.
-
The mechanism could involve (a) initial
vasoconstriction which leads to (b) acidosis, tissue ischemia, and
release those substances that themselves activate pain
receptors.
-
Increased pain therefore leads to increase
sympathetic outflow in the initiation of the cycle, sometimes called
reflex sympathetic dystrophy (complex regional pain syndrome(s) is
now the preferred designation).
-
Following some types of nerve injury, pain may occur without
requiring activation of pain receptors. That is, spontaneous
firing of injured peripheral nerves may occur and may be more
likely to occur in response to sympathetic nervous system
simulation.
-
The cardiovascular effects of pain involve four major systems:(1)
catecholamine release and sympathetic nerve terminals & adrenal
medulla (2) aldosterone & cortisol release from the adrenal
cortex and (3) antidiuretic hormone release from hypothalamus and
(4) activation of the renin-angiotensin system. Why should
these changes influence the cardiovascular system?
-
Increased angiotensin II promotes generalized
vasoconstriction, causing hypertension and increasing cardiac
work by increasing afterload
-
Catecholamines directly cause a positive chronotropic &
inotropic effect and increase systemic vascular resistance,
latter of which also increases afterload
-
Increase circulating catecholamines promote arrhythmias
directly as well as by exacerbating underlying myocardial
ischemia. [Recall that significant perioperative morbidity
is associated with myocardial dysfunction]
-
Increased aldosterone, cortisol, and ADH (antidiuretic
hormone) in concert with angiotensin II and catecholamine
effects all work in the direction of promoting congestive heart
failure, although this effect would be more likely patients with
intrinsically limited cardiac reserve. Accordingly,
preoperative assessment for the purpose of identification of
patients who may have limited cardiac reserve or some cardiac
dysfunction is particularly important as it also underscores the
necessity of effective clinical pain management.
Endocrine Effects associated with
Postoperative Pain
|
sodium
and water retention |
increased
protein catabolism |
hyperglycemia |
Immunological Effects associated with
Postoperative Pain
|
Reduce
Immune Function |
Coagulation System effects associated with
Postoperative Pain
|
Hypercoagulation
States* |
Deep
vein thrombosis |
Increased
platelet adhesiveness |
Reduced
fibrinolysis |
-
*Note: Epidural anesthesia reduces postoperative thromboembolic
complications; however, the underlying molecular mechanisms are not
completely understood.
-
In a recent study of major orthopedic
surgical procedures, general anesthesia was compared with local
anesthesia in terms of postoperative hypercoagulability states.
-
With
general anesthesia, orthopedic surgery induced a hypercoagulable
state, as assessed by increased platelet-mediated hemostasis time,
clotting time, and collagen-induced thrombus formation.
-
By
contrast, in the patient group receiving epidural anesthesia, these
parameters were not altered. Apparently, epidural anesthesia reduces
the likelihood of immediate post-operative hypercoagulability without
influencing physiologic aggregation and the coagulation process. (Hollmann MW, Wieczorek KS, Smart M, Durieux ME.,Reg Anesth Pain Med 2001 May;26(3):215-222.)
3General anesthesia even with parenteral
opioid administrationa has limited effect on postoperative
hypercoagulability.
-
3Coagulation effects are probably
related to stress-associated changes in (a) blood viscosity, (b)
platelet function, (c) fibrinolysis and (d) coagulation pathway
effects.
-
The consequences of these changes are manifest as increased
platelet adhesiveness, reduced fibrinolysis and the production of
a hypercoagulable state.
-
These coagulation effects, when taking in combination with
microcirculatory effects of increased circulating catecholamines,
are probably responsible for the increased incidence of
thromboembolism.
Gastrointestinal system effects associated
with Postoperative Pain
|
Ileus |
-
3Reduction in gastrointestinal
function would be expected based on sympathetic hyperactivity,
recalling that the parasympathetic system promotes motility, whereas
sympathetic action retards GI motility. The clinical
consequence of postoperative ileus include:
-
increased nausea, vomiting, generalized discomfort as well as
-
delay in resumption of enteral diet
-
3The delay in resumption of an enteral
diet itself may have adverse clinical effects (postoperative
morbidity) including an increase likely those septic complications
& abnormal wound healing.
Genitourinary system effects associated with
Postoperative Pain
|
Urinary
retention |

Acute Post-Operative Pain Management

Management of some pain syndromes
(Chronic, subspecialty anesthesia practice)
-
5Epidural steroid injection --
injection administration site is at the lesion level; e.g.L4-5 in
this case. Drawing from Warfield, C.A.:Manual of Pain
Management, p. 277, Philadelphia, Lippincott, 1991 obtained from
Aberle, K.L and Warfield, C.A. "Basis of Contemporary Pain
Management" in Principles and Procedures and Anesthesiology,
Philip L. Liu, editor, J. B. Lippincott Company, Philadelphia,
Chapter 23 p.368, 1992 (use by permission in secondary source)
-
6Root compression is more commonly
observed at the L5 and S1 levels due to anatomical factors (these
nerves pass through a relatively narrow lateral bony recess in
exiting the spinal canal.
-
Lumbosacral radiculopathy symptoms include:
-
low back pain with radiation to lower extremity (varying
distance)
-
consider disease, motor/sensory loss occurs
-
Although surgery may be indicated for large midline disk
involvement that manifests as bowel & bladder dysfunction,
initial treatment is usually limited to immobilization with mild
analgesics along with slow resumption of activity [prolonged
immobilization is unlikely to be helpful]
-
Therefore, only if conservative management (rest +analgesics)
fails to resolve pain would intervention with epidural steroids
be considered
-
As noted earlier, proper drug (steroid) localization is
inferred from immediate analgesia due to the concurrently
administered local anesthetic.
-
A concern mainly in patients with S1 radiculopathy is that
the drug will not spread adequately. Therefore caudal
injection may be more appropriate, perhaps utilizing a
radio-opaque catheter positioned using fluoroscopy.
-
Risk associated with epidural steroid injections: probably
extremely low based on reports in which usually 1-3 injections
have been used with 40-80 methylprednisolone acetate or 50 mg
triamcinolone diacetate
-
Corticosteroid doses used for management of radiculopathy,
however, are sufficient to suppress (acutely) the
hypothalamic-pituitary-adrenal (HPA) axis as evidenced by
reduced plasma cortisol and adrenocorticotropic hormone
level response to provocation.
-
As an example, when the treatment protocol required three
epidural triamcinolone injections at one-week
intervals, all patients recovered from HPA suppression
after three months.
-
A more significant suppression of
the HPA axis may be associated when midazolam (Versed)
was used for sedation. Altogether these findings
suggest that exogenous steroids might be appropriate for
patients undergoing significant stress during a
"vulnerable" period following epidural
steroid.
-
Furthermore, epidural steroid treatment
should be used with cautions in the diabetic patient because
(a) of increased epidural infection risk and (b) since
glucose control may be adversely affected.
-
Since immunosuppression will accompany epidural
steroid use, aseptic technique must be emphasized during
the procedure.
|