Medical Pharmacology Chapter 35 Antibacterial Drugs
The Aminopenicillins: Ampicillin and Amoxicillin
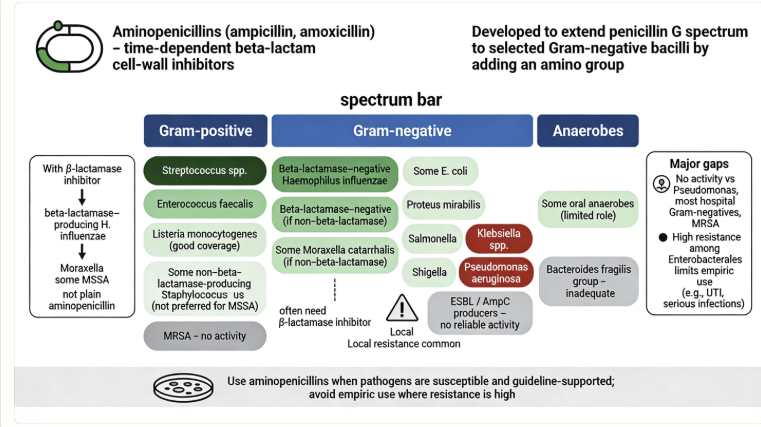 |
Ampicillin was initially developed (in the 1960s) to broaden penicillin’s spectrum to include more Gram-negative organisms and to allow oral administration.2
Spectrum
The aminopenicillins retain strong activity against many Gram-positive cocci, including Streptococcus pneumoniae, Streptococcus pyogenes (Group A strep), and other streptococci, as well as susceptible Enterococcus faecalis.3,4
Aminopenicilins have no activity against Staphylococcus aureus on their own if the strain produces penicillinase (the vast majority of S. aureus do), because the enzyme rapidly inactivates ampicillin/amoxicillin.
Listeria monocytogenes (a Gram-positive bacillus) is notably very susceptible to aminopenicillins which is a distinguishing feature, as these drugs penetrate host cells moderately well and can kill this intracellular pathogen.3
Aminopenicillins also cover certain anaerobes such as Clostridium species and Actinomyces (except C. difficile, which is inherently resistant), and they cover Corynebacterium spp. and other miscellaneous Gram-positives.3
Where aminopenicillins extended penicillin’s spectrum was in Gram-negative coverage.
These agents can penetrate the outer membrane of some Gram-negatives and resist stomach acid.
Organisms in the bowel and urinary tract such as non-β-lactamase-producing strains of Escherichia coli and Proteus mirabilis are typically susceptible .3
They also have activity against Salmonella and Shigella species (ampicillin can treat typhoid fever and shigellosis if the isolate is sensitive).4
Haemophilus influenzae is another Gram-negative target – ampicillin/amoxicillin can kill H. influenzae, but only if the strain does not produce beta-lactamase.3
Many wild-type H. influenzae were originally ampicillin-susceptible, but now >30% produce a penicillinase, making them resistant to aminopenicillins unless a β-lactamase inhibitor is added.
Aminopenicillins do not reliably cover Klebsiella, Enterobacter, Pseudomonas, Serratia, or Proteus vulgaris, among others – either due to intrinsic penicillinase production or other resistance factors.4
For instance, Klebsiella pneumoniae inherently produces a penicillinase that destroys ampicillin, so K. pneumoniae is considered intrinsically resistant.6
Pseudomonas aeruginosa is also intrinsically resistant; aminopenicillins cannot penetrate Pseudomonas’s outer membrane effectively and Pseudomonas has multiple efflux pumps and chromosomal AmpC β-lactamase.5
 |
|
Therefore, aminopenicillins are ineffective for pseudomonal infections (antipseudomonal penicillins like piperacillin are needed in that context).
The foremost mechanism of resistance to ampicillin/amoxicillin in community pathogens is beta-lactamase enzyme production, which cleaves the beta-lactam ring and inactivates the drug.2
Many Gram-negative bacteria (e.g. E. coli, H. influenzae, Moraxella, Proteus) commonly harbor plasmid-mediated beta-lactamases (like TEM-1) that confer resistance. This concern can be circumvented by combining the aminopenicillin with a beta-lactamase inhibitor, as described earlier, effectively extending coverage to beta-lactamase producing strains of those species.3
Another mechanism is alteration of PBPs: for example, penicillin-resistant Streptococcus pneumoniae has modified PBP structures (e.g. PBP2x and PBP2b changes) that lower affinity for all penicillins, including amoxicillin.7
Higher doses of amoxicillin (e.g. high-dose amoxicillin for otitis media or pneumonia) may still overcome intermediate pneumococcal resistance in some cases by achieving higher tissue concentrations.
Enterococcus faecium often exhibits resistance to ampicillin via a modified PBP (PBP5). The majority of E. faecium strains (especially hospital-associated ones) are ampicillin-resistant, whereas E. faecalis is usually ampicillin-susceptible.
Porin changes in Gram-negatives can also reduce entry of aminopenicillins into the periplasm.8
In summary, while aminopenicillins have a useful broad spectrum, resistance is now common in many organisms, and local susceptibility patterns must be considered.
Clinical use is often guided by whether the likely pathogens are beta-lactamase negative and known to be ampicillin-susceptible.
September, 2025
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |