|
|
|
Medical Pharmacology Chapter 33-34: Anticancer Drugs
Targeted Anticancer Drugs:
![]() Tyrosine Kinase Small Molecules Inhibitors in Cancer
Tyrosine Kinase Small Molecules Inhibitors in Cancer
![]() The introduction of targeted pharmacological
therapies has dramatically changed cancer treatment.
The introduction of targeted pharmacological
therapies has dramatically changed cancer treatment.
One example of such as targeted therapy are represented by tyrosine kinase inhibitors (TKIs).
Tyrosine kinases are central to many normal cellular processes; however, dysregulation associated with this enzyme is prominent in numerous cancers.
Dysregulation of tyrosine kinase may be due to mutations, overexpression of the enzyme, or chromosomal translocations. (5)
Abnormal tyrosine kinases represent an important therapeutic target.(6)
Tyrosine kinases
"Receptor Tyrosine Kinases: Phosphorylation of Proteins"
Attribution:
Henrik Receptor Tyrosine Kinases - RTK
https://www.youtube.com/watch?v=44iGSUrJYr8
Henrik's Lab
 |
|
Description and normal function
Tyrosine kinases (TKs) describe the family of enzymes catalyzing phosphate group transfer from ATP to tyrosine residues on particular proteins. This tyrosine phosphorylation is an important mechanism of signal transduction in mammalian cells.
Tyrosine kinases are important in regulating many cellular processes such as (7):
Cell growth and proliferation (control of cell-cycle and cell division).
Differentiation (Kinases are involved in specialized cellular functions).
Metabolism (Tyrosine kinases affect cellular metabolic pathways).
Apoptosis (also known as programmed cell death): Tyrosine kinases or are involved in some pathways triggering apoptosis.
Angiogenesis (new blood vessel formation): Tyrosine kinases are important in signaling pathways which promote new blood vessel growth which is important for tissue growth and repair.
Classes of tyrosine kinases (8):
Receptor Tyrosine Kinases (RTKs):
These proteins are described as transmembrane consisting of both an extracellular ligand-binding region, a transmembrane region, and an intracellular region that is responsible for kinase enzyme activity.
Binding of the biologically active ligand such as epidermal growth factor (EGF) or platelet-derived growth factor (PDGF) to the extracellular region results in receptor dimerization (two receptors coming together) as well as autophosphorylation of specific tyrosine amino acid residues in the intracellular region.
These processes result in docking sites for of subsequent, downstream signaling proteins resulting in the intracellular signaling cascade.
Signaling pathways belonging to this class include (8):
EGFR (Epidermal Growth Factor Receptor)
![]() The Epidermal Growth Factor Receptor (EGFR) is a
transmembrane glycoprotein that belongs to the ErbB
family of receptor tyrosine kinases (RTKs). (11)
The Epidermal Growth Factor Receptor (EGFR) is a
transmembrane glycoprotein that belongs to the ErbB
family of receptor tyrosine kinases (RTKs). (11)
EGFR plays a crucial role in normal cellular processes, including cell growth, proliferation, differentiation, survival, and migration.(11)
EGFR is activated upon binding of its specific ligands, such as epidermal growth factor (EGF) and transforming growth factor-alpha (TGF-α). (12)
Binding induces receptor dimerization, leading to autophosphorylation of tyrosine residues within the intracellular kinase domain.
This phosphorylation event then initiates a cascade of downstream signaling pathways, including the RAS/RAF/MEK/ERK (MAPK) pathway, the PI3K/AKT/mTOR pathway, and the STAT pathway.
These pathways ultimately regulate gene expression, promoting cellular functions essential for tissue development and homeostasis.
![]() EGFR and Cancer
Development
EGFR and Cancer
Development
Dysregulation of EGFR signaling is a common event in various human cancers, contributing significantly to tumorigenesis, progression, and metastasis. (13)
This dysregulation can occur through several mechanisms, including gene amplification, overexpression of the receptor, and activating mutations within the EGFR gene itself (11).
In the context of cancer, aberrant EGFR activation leads to:
Uncontrolled cell proliferation
Inhibition of apoptosis (programmed cell death)
Enhanced angiogenesis (formation of new blood vessels)
Increased metastatic potential (14).
The sustained activation of the downstream signaling pathways (MAPK, PI3K/AKT, STAT) provides a constant pro-growth and pro-survival signal to cancer cells, making them less dependent on external growth factors and more resistant to conventional therapies (11).
![]() Non-small cell lung cancer
(NSCLC) is a prime example where EGFR plays a
critical oncogenic role.
Non-small cell lung cancer
(NSCLC) is a prime example where EGFR plays a
critical oncogenic role.
Activating mutations in the EGFR gene are found in approximately 10-15% of NSCLC patients in Western populations and up to 50% in East Asian populations (15).
The most common EGFR mutations are deletions in exon 19 and a point mutation (L858R) in exon 21, which together account for about 90% of all activating EGFR mutations (15).
These mutations lead to constitutive (ligand-independent) activation of the EGFR kinase, driving tumor growth and survival (16).
The discovery of these EGFR activating mutations revolutionized the treatment of NSCLC.
Patients with these mutations are highly sensitive to EGFR tyrosine kinase inhibitors (TKIs), such as gefitinib, erlotinib, and osimertinib.
These drugs competitively bind to the ATP-binding site of the EGFR kinase domain, preventing autophosphorylation and subsequent activation of downstream signaling pathways.
This targeted approach has significantly improved response rates, progression-free survival, and quality of life for NSCLC patients harboring EGFR mutations compared to traditional chemotherapy (17).
HER2 (Human Epidermal Growth Factor Receptor 2)
Her2 Audio Overview
HER2 (Receptor Tyrosine-Protein Kinase erbB-2) and its Role in Cancer Development (35)
HER2, also known as receptor tyrosine-protein kinase erbB-2, is a protein encoded by the ERBB2 gene in humans.
HER2 is a member of the epidermal growth factor receptor (EGFR) family, which consists of four closely related receptor tyrosine kinases: EGFR (HER1/ErbB1), HER2 (ErbB2), HER3 (ErbB3), and HER4 (ErbB4).
These receptors play crucial roles in normal cell growth, differentiation, and survival by mediating signals from outside the cell to inside.
Unlike other HER family members, HER2 does not have a known direct ligand.
Instead, it acts as a preferred heterodimerization partner for other ligand-bound HER receptors, amplifying their signaling and contributing to a wide range of cellular processes.
Role in Cancer Development (36)
The ERBB2 gene amplification and subsequent overexpression of the HER2 protein are implicated in the development and progression of various human cancers, most notably breast cancer.
When HER2 is overexpressed, it leads to an uncontrolled activation of downstream signaling pathways, promoting cell proliferation, survival, angiogenesis, and metastasis.
Breast Cancer (37)
|
In breast cancer, HER2 amplification/overexpression occurs in approximately 15-20% of cases, defining a distinct subtype known as HER2-positive breast cancer.
This subtype is historically associated with more aggressive disease, higher rates of recurrence, and poorer prognosis compared to HER2-negative breast cancers. The overexpression of HER2 drives tumor growth through several key mechanisms:
Constitutive Activation: The high concentration of HER2 on the cell surface can lead to receptor dimerization and activation even in the absence of a ligand, resulting in continuous signaling.(21)
Enhanced Signaling: As a preferred heterodimerization partner, HER2 can form highly stable and potent signaling complexes with other HER family members (e.g., HER2-HER3 heterodimers are particularly strong activators of the PI3K/Akt pathway).
Activation of Downstream Pathways: The activated HER2 receptor phosphorylates intracellular tyrosine residues, which serve as docking sites for adaptor proteins.
This activation initiates a cascade of intracellular signaling pathways, primarily the mitogen-activated protein kinase (MAPK) pathway and the phosphoinositide 3-kinase (PI3K)/Akt pathway.
MAPK Pathway: Activation of this pathway leads to changes in gene expression that promote cell proliferation and survival.
PI3K/Akt Pathway: This pathway is critical for cell survival, growth, and inhibition of apoptosis.
Its dysregulation is a common feature in many cancers.
Clinical Significance and Therapeutic Targeting
![]() The
discovery of HER2's oncogenic role revolutionized
the treatment of HER2-positive breast cancer.
The
discovery of HER2's oncogenic role revolutionized
the treatment of HER2-positive breast cancer.
HER2 status is a critical biomarker determined through immunohistochemistry (IHC) and/or fluorescence in situ hybridization (FISH) tests.
Patients with HER2-positive breast cancer are eligible for HER2-targeted therapies, which have significantly improved outcomes.
The most prominent example of a HER2-targeted therapy is trastuzumab (Herceptin) (38), a monoclonal antibody that binds to the extracellular domain of the HER2 protein, preventing its dimerization and signaling, and also mediating antibody-dependent cell-mediated cytotoxicity (ADCC).
Other HER2-targeted agents include pertuzumab (another monoclonal antibody that prevents HER2 dimerization), lapatinib and neratinib (tyrosine kinase inhibitors that block the intracellular kinase domain), and antibody-drug conjugates like T-DM1 (trastuzumab emtansine).
These therapies, often used in combination with chemotherapy, have transformed HER2-positive breast cancer from a highly aggressive disease into one with increasingly favorable prognoses.
VEGFR (Vascular Endothelial Growth Factor Receptor)
PDGFR (Platelet-Derived Growth Factor Receptor)
![]() Non-Receptor Tyrosine Kinases (nRTKs):
(39)
Non-Receptor Tyrosine Kinases (nRTKs):
(39)
These are cytoplasmic or nuclear proteins that lack a transmembrane domain.
They are often activated downstream of RTKs or by other cellular signals, such as those from integrins or cytokine receptors.
nRTKs also play vital roles in various signaling pathways.
Examples include:
![]() ABL1
(Abelson murine leukemia viral oncogene homolog 1) (10):
ABL1
(Abelson murine leukemia viral oncogene homolog 1) (10):
ABL1 (tyrosine-protein kinase ABL1) is protein encoded by the ABL1 gene located on chromosome 9.
The ABL1 proto-oncogene encodes of cytoplasmic and nuclear protein tyrosine kinase likely involved in cell division, cell differentiation, cell adhesion and DNA repair.
Mutations in the ABL1 gene are important in the development of chronic myelogenous leukemia (CML).
In CML, ABL1 is activated following translocation within the BCR (breakpoint cluster region) gene on chromosome 22.
This activity results in the new fusion gene, BCR-ABL, which encodes an unregulated tyrosine kinase protein which promotes cellular proliferation absent regulation by cytokines.
The cell as result has become cancerous (9)
 |
|
SRC (SaRComa)
Src is an example of the proto-oncogene tyrosine protein kinase (a.k.a. Proto-oncogenec-Src or c just c-Src), classified as a non-receptor tyrosine kinase. (18)
Activation of the c-SRC pathway has been described in about 50% of tumors from:, liver, breast, lung and pancreas.
Activation of c-SRC results in enhanced cellular survival, angiogenesis, proliferation as well as aberrant tumor growth in cancers.
![]() The
likely mechanism is development of genetic mutations
that increase either the activity or promote
overexpression of c-SRC, resulting in constant
activation of c-SRC.(18)
The
likely mechanism is development of genetic mutations
that increase either the activity or promote
overexpression of c-SRC, resulting in constant
activation of c-SRC.(18)
JAK (Janus Kinase),
Janus refers to the two-faced Roman god due to the presence of the second phosphotransferase located opposite the first). (19)
Janus kinase (JAK) describes the family of non-receptor tyrosine kinases that transduce cytokine-mediated input via the JAK-STAT pathway.
JAK family members include Janus kinase 1, Janus kinase 2, Janus kinase 3 and tyrosine kinase 2.
Janus kinase 1 has been identified as both critical for pancreatic cancer initiation and progression. (20)
Most pancreatic ductal adenocarcinomas develop as result of gain-of-function mutations in K-ras as well as epigenetic alterations.
![]() Dysregulation
of Tyrosine Kinase is in Cancer
Dysregulation
of Tyrosine Kinase is in Cancer
The tightly regulated activity of tyrosine kinases is essential for maintaining cellular homeostasis. However, in many cancers, these enzymes become dysregulated, leading to uncontrolled cell signaling that drives tumor development and progression. Mechanisms of TK dysregulation in cancer include:
Mutations: Genetic mutations can lead to constitutive (continuous) activation of TKs, meaning they are "switched on" even in the absence of normal activating signals.
For example, mutations in the EGFR gene are common in non-small cell lung cancer (NSCLC). (22)
Gene Amplification: An increase in the number of copies of a TK gene can lead to overexpression of the kinase, resulting in excessive signaling. (23)
Amplification of HER2 (ERBB2) in breast cancer is a prominent example.
Chromosomal Translocations: These can create fusion genes that encode constitutively active chimeric tyrosine kinases. (24, 25)
![]() The
Philadelphia chromosome, resulting from a translocation between chromosomes
9 and 22, creates the BCR-ABL fusion protein, which is characteristic of
chronic myeloid leukemia (CML).
The
Philadelphia chromosome, resulting from a translocation between chromosomes
9 and 22, creates the BCR-ABL fusion protein, which is characteristic of
chronic myeloid leukemia (CML).
Overexpression of Ligands or Receptors: Increased production of growth factors or their corresponding RTKs can also lead to hyperactivation of signaling pathways (26).
Aberrant TK activity contributes to several "hallmarks of cancer," including sustained proliferative signaling, evasion of growth suppressors, resistance to cell death, induction of angiogenesis, and activation of invasion and metastasis.
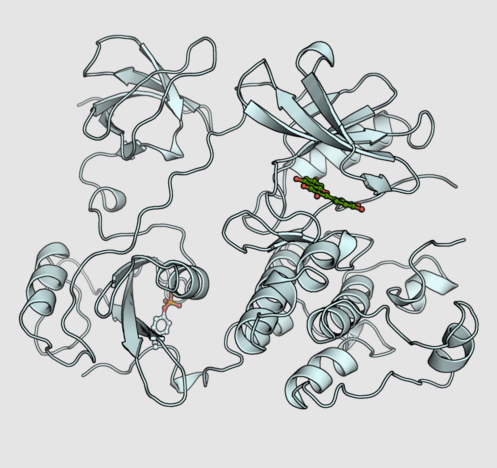
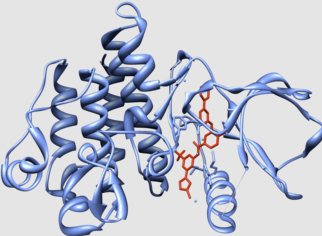
Tyrosine Kinase Inhibitors (TKIs): Mechanism of Action (27)
Small molecule tyrosine kinase inhibitors (TKIs) are designed to block the activity of these dysregulated kinases.
Most TKIs are ATP-competitive inhibitors, meaning they bind to the ATP-binding pocket of the kinase domain.
By occupying this site, they prevent ATP from binding, thereby inhibiting the phosphorylation of substrate proteins and blocking downstream signaling pathways.
TKIs can be classified based on their selectivity:
Selective TKIs: Target one or a few specific tyrosine kinases.
Multi-targeted TKIs: Inhibit a broader range of different tyrosine kinases.
Use of TKIs in Cancer Therapeutics
Imatinib (Gleevec): This was one of the first highly successful TKIs. (28)
Imatinib targets the BCR-ABL fusion protein in CML, as well as KIT and PDGFR.
This drug has dramatically improved the prognosis for CML patients, converting a once fatal disease into a manageable chronic condition for many .
Imatinib is also used for gastrointestinal stromal tumors (GIST) harboring KIT mutations.
Gefitinib (Iressa) and Erlotinib (Tarceva): These are first-generation EGFR TKIs used to treat NSCLC patients whose tumors have activating mutations in the EGFR gene. (29)
These drugs have shown significant efficacy in this molecularly defined subgroup.
Osimertinib (Tagrisso): A third-generation EGFR TKI, osimertinib is effective against NSCLC with specific EGFR mutations, including the T790M resistance mutation that can develop after treatment with first or second-generation EGFR TKIs. (30)
Sunitinib (Sutent) and Sorafenib (Nexavar): These drugs are multi-targeted TKIs that inhibit VEGFR, PDGFR, and other kinases. (31, 32)
They are used in the treatment of renal cell carcinoma (kidney cancer), hepatocellular carcinoma (liver cancer), and GIST.
Crizotinib (Xalkori): This TKI targets ALK (anaplastic lymphoma kinase) and ROS1 fusion proteins found in some NSCLCs, leading to significant tumor responses. (33)
Lapatinib (Tykerb): Targets both EGFR and HER2, used in HER2-positive breast cancer, often in combination with chemotherapy.(34)