Medical Pharmacology Chapter 35 Antibacterial Drugs
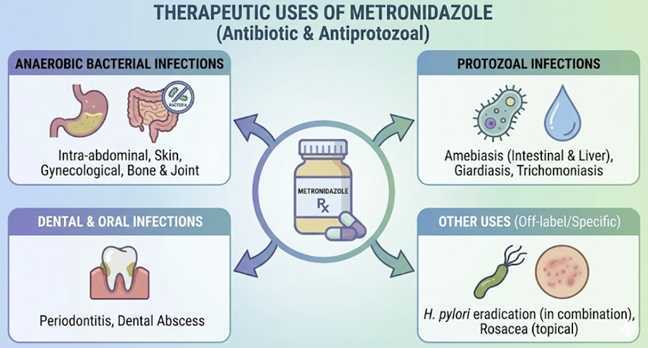
Anaerobic Bacteria Infections and Others: Metronidazole Therapeutic Uses
 |
Intra-abdominal infections including perforated appendicitis, diverticulitis abscess, or peritonitis may benefit from metronidazole administration.1
In this case, recognizing that such infections may be polymicrobial, metronidazole is often administered as part of regimen including drugs that cover Gram-negative aerobes (e.g. a fluoroquinolone or cephalosporin).2
An outpatient regimen for mild diverticulitis is commonly ciprofloxacin + metronidazole, though current guidelines also allow amoxicillin-clavulanate monotherapy.3
Abscesses in the abdomen, liver, brain, or lung often require metronidazole as part of therapy because of the presence of anaerobes.4
In lung abscess (where mouth anaerobes like Prevotella and Fusobacterium are implicated), metronidazoleis not useful as monotherapy.
Preferred, initial empiric antibiotic therapy include the use of beta-lactamase inhibitor combination such as ticarcillin-clavulanate, amoxicillin-clavulanate, or piperacillin-tazobactam.
![]() Amoxicillin-clavulanate
represents the drug of choice for oral antibiotics to treat lung
abscess.5
Amoxicillin-clavulanate
represents the drug of choice for oral antibiotics to treat lung
abscess.5
In aspiration pneumonia, metronidizole would be most likely appropriate in those patients with evidence of lung abscess, necrotizing pneumonia, putrid sputum or severe periodontal disease.6
In a recent multicenter retrospective cohort study, data interpretation suggested that extended anaerobic coverage was likely unnecessary and aspiration pneumonia because it was associated with no additional mortality benefit, "only an increased risk of C. difficile colitis.7
It is effective in postpartum endometritis when Bacteroides, one of the anaerobic bacteria involved in this infection, frequently in combination with other antibiotics.
Metronidazole is also the drug of choice for anaerobic infections of the central nervous system (brain abscess, subdural empyema) because of its excellent CSF penetration.1
Additionally, it is used for skin and soft tissue infections caused by anaerobes.8
In colorectal surgery prophylaxis, IV metronidazole with cefuroxime is one effective combination to prevent surgical site infections by gut anaerobes.9
Gynecologic and Genitourinary Infections
Metronidazole is first-line therapy for bacterial vaginosis (BV), an anaerobe-associated vaginal infection.10
The CDC’s 2021 STI treatment guidelines continue to recommend metronidazole 500 mg orally twice daily for 7 days as the preferred BV regime (an intravaginal metronidazole gel for 5 days is an alternative).10
This treatment alleviates symptoms and may reduce the risk of pelvic inflammatory disease.11
Metronidazole is also indicated for trichomoniasis, a common sexually transmitted infection (protozoal).12
Updated guidelines have modified trichomoniasis therapy: for women (including pregnant women), a 7-day course of metronidazole 500 mg BID is now recommended over a single dose, due to improved cure rates.12
For men with trichomoniasis, a single 2 g dose is still recommended, as men are typically asymptomatic carriers).12
Another important use is in Pelvic Inflammatory Disease (PID).13
Current guidelines always include parenteral or oral metronidazole as combination therapy in outpatient PID regimens to ensure anaerobic coverage (particularly to cover Bacterial vaginosis (BV) organisms and Prevotella that often accompany gonococcal/chlamydial pelvic inflammatory disease.13
For example, the CDC recommends IM ceftriaxone plus doxycycline plus metronidazole 500 mg BID for 14 days for PID management.14
The metronidazole component treats anaerobes and G. vaginalis, improving clinical cure and reducing tubo-ovarian abscess risk.15
Metronidazole (among other antibiotics) is also used for endometritis, post-abortal infections, and septic miscarriage in combination regimens.16
In the male GU sphere, metronidazole can treat prostatitis or epididymitis when caused by anaerobes (for example Trichomonas vaginalis).17
Gastrointestinal Protozoal Infections
Metronidazole is a mainstay for intestinal parasites.18,19,20
For giardiasis, acquired from contaminated water or food causing diarrhea and malabsorption, metronidazole (250 mg TID for 5–7 days in adults) is effective.21 A report is indicated failure rates with metronidizole of up to 40% in clearing parasites from the gut in addition to an issue with poor patient compliance.20
Metronidazole use is a common scenario in travel medicine or pediatrics (note: tinidazole, a related nitroimidazole, can be given as a single dose for Giardia and is equally effective but metronidazole remains widely used and inexpensive).21
For amebic dysentery or amebic liver abscess caused by E. histolytica, metronidazole is the first-line tissue amoebicide: a typical course is 750 mg TID for 7–10 days.22
This reliably kills the invasive trophozoites in the bowel wall and liver. However, because metronidazole does not eliminate dormant cysts in the intestine, patients must receive a luminal amebicide (such as iodoquinol or paromomycin) after the metronidazole course to prevent relapse.22
In practice, a primary care provider might see a returning traveler with bloody diarrhea and liver abscess on imaging – if diagnosed with amebiasis, the provider would hospitalize or or closely manage the patient with metronidazole followed by a luminal agent per CDC guidelines.22
Helicobacter pylori Infection
Metronidazole plays an integral role in several combination regimens for H. pylori, the gastric bacterium linked to peptic ulcers.23
While many H. pylori strains have metronidazole resistance, the drug is still included in bismuth-based quadruple therapy, which is a recommended first-line treatment, especially if clarithromycin resistance is a concer.24.
According to the American College of Gastroenterology’s 2024 guideline update, the preferred empiric regimen for H. pylori in many patients is 14-day bismuth quadruple therapy: a PPI + bismuth + tetracycline + metronidazole 500 mg (typically QID).24
This regimen achieves high eradication rates even in the face of clarithromycin or metronidazole resistance, by using multiple agents.24
In practice, a primary care physician diagnosing H. pylori in a patient with duodenal ulcer might prescribe this quadruple therapy (e.g. omeprazole, bismuth subsalicylate, tetracycline, and metronidazole) for 2 weeks.24
If the patient cannot tolerate one component, alternative regimens (like amoxicillin + metronidazole with a different acid blocker like vonoprazan) are options, but non-clarithromycin regimens are emphasized in recent guidelines due to resistance.24
Metronidazole is also part of H. pylori salvage regimens after initial failure – e.g. levofloxacin-based or rifabutin-based therapies may include metronidazole as well
Older triple therapy (PPI + clarithromycin + metronidazole) is now rarely used unless local resistance patterns are favorable.
Summary: Metronidazole remains a component of first-line therapy for H. pylori (in quadruple regimens) and is an important tool in ensuring eradication of this infection which primary care and GI clinicians commonly encounter.24
Clostridioides difficile (Also known as Clostridium difficile) Infection
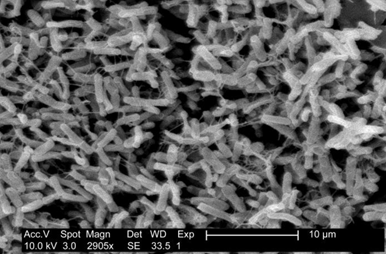 |
|
Historically, metronidazole was the first-line therapy for mild to moderate C. difficile colitis (antibiotic-associated diarrhea).
Response rates for C. difficile have declined (likely due to increasing resistance and the emergence of hypervirulent strains).25
Reduced susceptibility of C. difficile isolates has been reported, corresponding to higher recurrence rates.26
Because of this finding, recent guidelines have de-emphasized metronidazole monotherapy in C. difficile infection.
In 2017, the Infectious Diseases Society of America (IDSA) changed guidelines to recommend vancomycin or fidaxomicin over metronidazole as first-line treatment for adult C. difficile infection, even in non-severe cases.27,28
The latest IDSA focused update (2021) goes further: fidaxomicin is preferred, with vancomycin as alternative, and metronidazole is no longer recommended as sole therapy except in certain mild initial cases when other agents are unavailable.29
For example, in a resource-limited setting or if the patient cannot obtain oral vancomycin or fidaxomicin, metronidazole 500 mg TID for 10–14 days can be used for a first episode of mild C. difficile colitis.30
Metronidazole is still recommended as an adjunct IV therapy in fulminant C. difficile (where oral vancomycin is given for intraluminal effect, and IV metronidazole is added to treat systemic or ileus cases).30
In pediatric C. difficile, guidelines allow metronidazole or vancomycin for non-severe cases.28
In summary, primary care providers should be aware that while metronidazole was once a perferred drug for C. diff, current practice is to reserve it for select situations.
August, 2025
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. , This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |