Medical Pharmacology Chapter 35 Antibacterial Drugs
The Aminopenicillins: Ampicillin and Amoxicillin
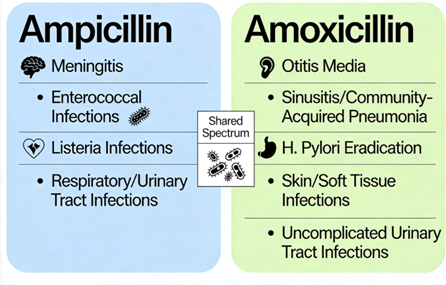 |
Some Therapeutic Uses
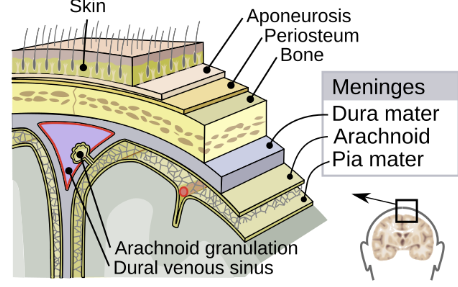
Meningitis and
CNS Infections
 |
|
 |
|
Ampicillin is an important antibiotic in the treatment of certain forms of bacterial meningitis.
While third-generation cephalosporins (e.g. ceftriaxone or cefotaxime) are the mainstay for most community-acquired bacterial meningitis (covering S. pneumoniae, N. meningitidis), there is one prominent pathogen that cephalosporins do not cover: Listeria monocytogenes.3
Listeria primarily causes meningitis in neonates, the elderly (>50 years), pregnant women, and immunocompromised hosts, and it is intrinsically resistant to cephalosporins.2
Ampicillin (or penicillin G) is the drug of choice for Listeria infections, including meningitis.2
WHO guidelines for bacterial meningitis recommend adding ampicillin to the empiric regimen whenever Listeria is a consideration.4 Often an aminoglycoside (gentamicin) is added to ampicillin for Listeria meningitis in severe cases to achieve synergy, though definitive evidence of improved outcomes with gentamicin is limited.2 Gentamicin is often part of initial therapy (along with e.g. ampicillin) for Listeria.2
An alternative for Listeria coverage, for example in the presence of penicillin allergy, is trimethoprim-sulfamethoxazole, as it penetrates the CSF and is listericidal.
Meropenem is another alternative.2
Aside from Listeria, ampicillin is active against many other meningeal pathogens.
Ampicillin covers Group B Streptococcus (Streptococcus agalactiae), a cause of neonatal meningitis, and is often included (with gentamicin) in empiric neonatal meningitis regimens.5
It also covers Neisseria meningitidis, Escherichia coli, non-beta-lactamase H. influenzae.
Penicillin or ampicillin can be used to treat susceptible N. meningitidis meningitis.
Ampicillin’s ability to penetrate the CSF is good when the meninges are inflamed5, achieving bactericidal concentrations.
Because up to ~30% of H. influenzae strains produce beta-lactamase and because penicillin-resistant pneumococci exist, the standard of care in meningitis is to use ceftriaxone (which covers those) plus vancomycin (for resistant pneumococci), and add ampicillin specifically for Listeria coverage when indicated.2
In summary, ampicillin is indispensable for Listeria meningitis and would be included in empiric therapy for meningitis in neonates and older adults.2
Ampicillin penetrates well into brain abscesses and cerebrospinal fluid with inflammation, so it may be used for Listeria brain abscess.6
Endocarditis and Enterococcal Infections
|
Ampicillin is useful in treating enterococcal infections, including endocarditis and enterococcal bacteremia.8,9
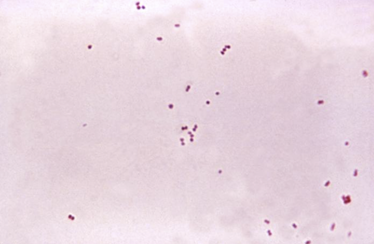
Enterococcus faecalis is a Gram-positive coccus inherently resistant to many antibiotics, but it is usually susceptible to ampicillin, unlike E. faecium, which is often ampicillin-resistant.6,7
 |
|
Ampicillin is may be bacteriostatic by itself against enterococci in vitro , meaning it inhibits growth but often does not rapidly kill the organisms.10
Serious enterococcal infections like endocarditis (infection of heart valves), bacteriostatic activity is not sufficient thus necessitating bactericidal combinations.
![]() Standard therapy for
Enterococcus faecalis endocarditis is
ampicillin combined with an aminoglycoside (gentamicin)
or cephalosporin (ceftriaxone) to achieve
bactericidal synergy.11
Standard therapy for
Enterococcus faecalis endocarditis is
ampicillin combined with an aminoglycoside (gentamicin)
or cephalosporin (ceftriaxone) to achieve
bactericidal synergy.11
Ampicillin damages the cell wall and may facilitate gentamicin entry into the bacterial cell, together proeducing a bactericidal effect.12
Clinical guidelines (American Heart Association and IDSA) traditionally recommended ampicillin (or aqueous penicillin G) plus gentamicin for enterococcal endocarditis for 4–6 weeks.13
This regimen cures most E. faecalis endocarditis, but gentamicin can cause nephrotoxicity and ototoxicity, and some enterococcal strains have high-level aminoglycoside resistance (HLAR).
Other current clinical guidelines suggest combining ampicillin with other agents e.g. ceftriaxone or daptomycin etc.14
Enterococcal bacteremia management begins with
identifying and controlling the source, which is most
often the urinary tract, an intra-abdominal process, or
an infected intravascular catheter.
For uncomplicated bacteremia where the source is
controlled (e.g., catheter removal), a treatment
duration of 7 to 14 days is generally sufficient.
Allergic reactions
Amoxicillin and ampicillin can cause hypersensitivity reactions in susceptible individuals.
These reacttopms range from mild rashes to severe anaphylaxis.
Penicillin allergy is the most important contraindication,
Any patient with a history of penicillin anaphylaxis should not receive aminopenicillins, due to risk of IgE-mediated reaction.19 Typical allergic manifestations include urticaria (hives), angioedema, pruritus, and wheezing or anaphylactic shock in severe cases.19
Aminopenicillins can also cause delayed hypersensitivity rashes that are not IgE-mediated.20
An example is ampicillin/amoxicillin rash in patients with viral infections: when ampicillin or amoxicillin is administered during acute Epstein-Barr virus (mononucleosis) infection, a high proportion of patients develop a non-allergic generalized maculopapular rash.21
A case report suggests that aminopenicillins may trigger characteristic rashes after the onset of mononucleosis, even when given during the infections latent phase.22
This “ampicillin rash” is immunologically distinct from a true penicillin allergy and does not preclude future use of penicillins, but it is a well-known reaction.23
Amoxicillin/ampicillin are generally avoided in patients with mononucleosis as these drugs may induce a pruritic erythematous maculopapular skin rash.24
Gastrointestinal Effects
Aminopenicillins are associated with GI side effects.
Adverse effects include diarrhea, nausea, and vomiting.
Ampicillin frequently causes diarrhea when given orally.25
Amoxicillin and ampicillin can cause changes in the gut microbiome that lead to superinfections: for instance, overgrowth of Candida yeasts (oral thrush or vaginal yeast infection) or Clostridioides difficile colitis.26
Antibiotic-associated diarrhea can occur with aminopenicillins, and in some cases severe C. difficile–associated diarrhea (pseudomembranous colitis) has been reported.19,26
September, 2025
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |