Medical Pharmacology Chapter 35 Antibacterial Drugs
The Isoxazolyl Penicillins: Oxacillin, Cloxacillin and Dicloxacillin
Isoxazolyl Penicillins Audio Overview
 |
 |
 |
 |
 |
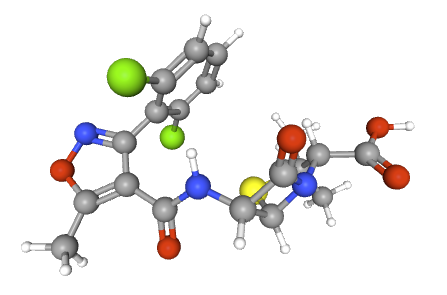 |
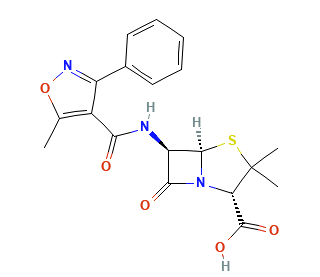
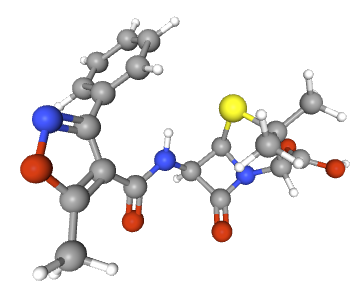
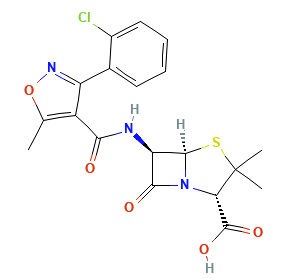
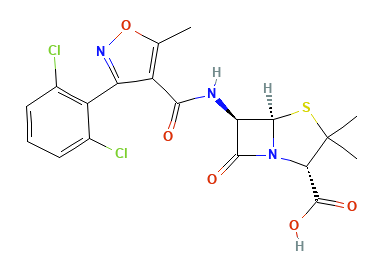
Oxacillin, cloxacillin, and dicloxacillin are narrow-spectrum β-lactams built for Methicillin-Susceptible Staphylococcus aureus (MSSA) and other penicillinase-producing staphylococci, with activity against β-hemolytic streptococci.1,2
These agents have no activity against MRSA (PBP2a/mecA), Enterococcus, anaerobes, or typical Gram-negative bacteria.1,6
![]() Oxacillin,9 cloxacillin,7 dicloxacillin8
or flucloxacillin7 provide
therapy of
Methicillin-Sensitive Staphylococcus aureus (MSSA) infections
across the severity spectrum:
Oxacillin,9 cloxacillin,7 dicloxacillin8
or flucloxacillin7 provide
therapy of
Methicillin-Sensitive Staphylococcus aureus (MSSA) infections
across the severity spectrum:
Oral dicloxacillin or cloxacillin for mild skin/soft-tissue disease.1 IV nafcillin might also be used.1
IV oxacillin for serious invasive disease such as bacteremia, endocarditis, osteoarticular infection, and device-associated infections when the isolate is MSSA.10
Guidelines for Skin and Tissue Infection (SSTI) and endocarditis place an antistaphylococcal penicillin (oxacillin/nafcillin) as first-line therapy for MSSA.11
Mechanism of Action and Resistance
Mechanisms of Action
Like all β-lactams, these agents covalently acylate penicillin-binding proteins (PBPs), blocking D-Ala-D-Ala–dependent transpeptidation and weakening peptidoglycan cross-linking which is bactericidal during active cell wall synthesis.12
Their bulky side chains sterically hinder many staphylococcal penicillinases, preserving activity against penicillinase-producing MSSA.12
MRSA resistance via altered target PBPs (PBP2a/PBP2′) encoded by mecA, not by penicillinase. Therefore these agents are inactive against MRSA.12,13
The mecA gene encodes PBP2a, a modified penicillin-binding protein that has a greatly reduced affinity for β-lactam antibiotics, allowing cell wall synthesis to proceed even in the presence of these drugs.14,15,16
MRSA and other mecA-positive staphylococci are resistant to all β-lactams, including penicillinase-resistant penicillins.
This is the dominant resistance mechanism in healthcare and community settings.
Detection of the mecA gene or its product PBP2a is essential for identifying MRSA.
Oxacillin
Oxacillin demonstrates rapid but incomplete absorption when administered orally, though the oral formulation is not available in the United States.
Following intravenous administration, peak serum concentrations are achieved within approximately 5 minutes.
A 500 mg slow intravenous dose produces peak levels of 43
The drug exhibits extensive protein binding, primarily to albumin, with reported binding rates of 94.2 ± 2.1%.
Oxacillin is widely distributed throughout body tissues and fluids, achieving therapeutic concentrations in pleural, bile, and amniotic fluids.
However, penetration into cerebrospinal fluid and ascitic fluid remains insignificant under normal conditions.17,19
Elimination occurs through multiple pathways, with approximately 30% excreted unchanged in urine via glomerular filtration and active tubular secretion.
The elimination half-life is approximately 0.5 hours in patients with normal renal function.
Nonrenal elimination includes hepatic inactivation and biliary excretion.17,18
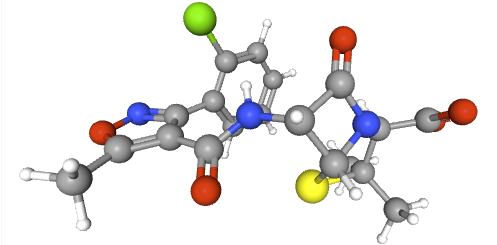
Dicloxacillin
Dicloxacillin exhibits superior oral bioavailability compared to other penicillinase-resistant penicillins.
The absolute bioavailability ranges from 35-76% when calculated from area under the curve data, with individual variations noted.
Peak serum concentrations (Tmax) are typically achieved within 0.75-1.25 hours following oral administration.20,21
The pharmacokinetic profile demonstrates dose-proportional increases in both maximum concentration (Cmax ) and area under the curve (AUC).
For doses ranging from 0.25 g to 2.0 g, Cmax values increase proportionally from 13.62 to 79.97 μg/mL.
The elimination half-life averages 1.51 hours and remains independent of dose.17,20,21
Dicloxacillin shows extensive protein binding, though specific values vary among studies.
Distribution is widespread throughout body tissues, with minimal penetration into cerebrospinal fluid except in the presence of meningeal inflammation.
Renal excretion accounts for 38-50% of the administered dose within 24 hours.18,20,22,23
The primary indication for these antibiotics includes treatment of serious staphylococcal infections such as bacteremia, endocarditis, pneumonia, and deep-seated abscesses.25,26
β-lactam antibiotics, including antistaphylococcal penicillins, appear superior to vancomycin for definitive therapy of MSSA bloodstream infections.24
Skin and Soft Tissue Infections
Dicloxacillin is commonly prescribed for outpatient treatment of staphylococcal skin infections, including impetigo, cellulitis, folliculitis, and wound infections.5
Penicillin-susceptible Staphylococcus aureus (PSSA) accounts for approximately 9% of pediatric skin and soft tissue infections, often requiring more intensive treatment including hospitalization and surgical intervention.27
Oxacillin and nafcillin are frequently used for treatment of osteomyelitis and septic arthritis caused by MSSA.6,28
In pediatric osteoarticular infections, there has been an increasing trend toward penicillin susceptibility among MSSA isolates, with PSSA accounting for 6.7% of cases in recent studies.27
Nafcillin is particularly favored for treatment of MSSA endocarditis, though recent research suggests that the presence of an inoculum effect in certain MSSA strains may influence treatment outcomes.
The choice between antistaphylococcal penicillins and cefazolin for endocarditis treatment continues to be debated, with some evidence suggesting superior outcomes with specific β-lactam agents.25
β-Lactam antibiotics are favored
over vancomycin or daptomycin for MSSA.29
September, 2025
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |