|
|
|
Autonomic Pharmacology--Adrenergic Drugs
|
|
|
|
Adrenergic Receptor Subtypes continued: Three subtypes of β-adrenergic receptors have been described: β1, β2, and β3.9
Activation of these receptors by agonist ligands cause activation of the stimulatory G protein, Gs, (as noted earlier, certain G proteins are inhibitory). Gs increases adenylyl cyclase catalytic activity which results in elevation of intracellular cAMP.
Higher levels of cAMP in turn promote phosphorylation of various proteins; the phosphorylation step changes protein function and thus is an important regulatory step.
cAMP is the primary second messenger system for the β-adrenergic receptor system and activation of the receptor system can cause, via cAMP, numerous tissue-specific effects.
![]()
One example is activation of glycogen phosphorylase in the liver secondary to β-adrenergic receptor induced [cAMP] elevation ([ ] refers to molar concentration).
In the kidney, β1-adrenergic receptor stimulation results in increased renin release; whereas, β1-cardiac adrenergic receptor stimulation increases both contractility and heart rate (positive inotropism and positive chronotropism respectively).
The positive chronotropic effect occurs because of the change in the slope of phase 4 spontaneous depolarization at sinoatrial nodal pacemaker cells.
The positive inotropic effect of adrenergic agonists occurs due to increased phosphorylation of Ca2+ ion channels.
In addition to enhanced sarcolemmal Ca2+-channel phosphorylation, β1-adrenergic activation also phosphorylates an important regulatory protein of the cardiac muscle Ca2+ calcium channel, phospholamban.40
Phospholamban, when acted on by protein kinase A, an effects stimulated by cAMP secondary to β1-adrenergic receptor activation, becomes phosphorylated and then exhibits a reduced ability to inhibit a sarcoplasmic reticulum calcium pump (SERCA2).
Therefore, the phosphorylated phospholamban increases activity of this Ca2+ pump, consequence of which is to both reduce free Ca2+ (this favors cardiac muscle relaxation in diastole) and increase the amount of Ca2+ calcium released from sarcolemmal stores with the next action potential.40
This latter action results in the positive inotropic effect observed following phospholamban phosphorylation. (More detailed studies of the phospholamban phosphorylation pattern indicate three protein kinase-dependent phosphorylation sites:
(1) the cAMP-dependent protein kinase just described phosphorylates a serine amino acid residue,
(2) a Ca2+/calmodulin-dependent protein kinase catalyzes a phosphorylation reaction at a threonine amino acid residue and
(3) protein kinase C catalyzes phosphorylation of a distinct serine amino acid residue. These phosphorylation reactions all appear to stimulate initial rates of sarcoplasmic reticulum Ca2+-transport.40
Dephosphorylation of phospholamban is catalyzed by a cardiac sarcoplasmic reticulum-associated type 1 protein phosphatase, which is also controlled by cAMP-dependent phosphorylation of its inhibitor protein.40
 |
With respect to possible clinical correlation, heart failure (CHF, congestive heart failure) is a disease associated with abnormal intracellular Ca2+-"handling." Specifically, cardiac relaxation and rapid reduction of cytosolic [Ca2+] by SERCA2 appear impaired with a resulting increase in diastolic [Ca2+]. Such an increase, by reducing cardiac sarcoplasmic reticulum stores, reduces Ca2+ availability for subsequent cardiac contractions. Possible clinical therapeutic approaches might involve altering phospholamban or SERCA2 protein expression levels or disruption of the phospholamban-SERCA2 complex.40
The combination of β1-adrenergic receptor mediated increases in both heart rate and contractility (positive inotropism) results in an increase in cardiac output.
Changes in conduction velocity at the atrioventricular (AV) node are also mediated by β1 receptors: 9
(1) Activation of these receptors increases conduction velocity by increasing Ca2+-channel conductance. Depolarization of AV nodal cells is especially sensitive to Ca2+ because in this specialized cardiac tissue Ca2+ as opposed to Na+ provides the primary inward, depolarizing current.
(2) Therefore, by contrast, blockers or antagonists that act at β1-receptors decrease conduction through the AV node.
Short-acting β-receptor antagonists, such as esmolol, ( β1-receptor selective) may be helpful in rapid, short-term management of high ventricular following rates in the setting of supraventricular arrhythmias (e.g. atrial fibrillation).
|
|
|
|
|
The recognition that β1-receptors promote increases in both heart rate and myocardial contractility presents opportunities for pharmacological management of several cardiovascular disorders, including hypertension and angina.9
A reduction in blood pressure would be expected with β-adrenergic receptor antagonism because heart rate and force of contraction decrease.
Angina is a clinical symptom associated with an imbalance between myocardial oxygen requirements and oxygen availability.
If oxygen availability is limited by suboptimal coronary perfusion secondary, for example, to coronary atherosclerosis, one option is to decrease myocardial oxygen demand, by decreasing myocardial contractility.
Myocardial oxygen extraction is about 70% at rest (dog model).42, 42a Therefore, increased myocardial oxygen consumption must be accompanied by an increase in coronary blood flow, since there is limited additional oxygen extraction possible.
The relationship between coronary blood flow and myocardial oxygen consumption is approximately linear.42
|
|
Anatomical overview: large epicardial branches of the left and right coronary arteries undergo additional branching.
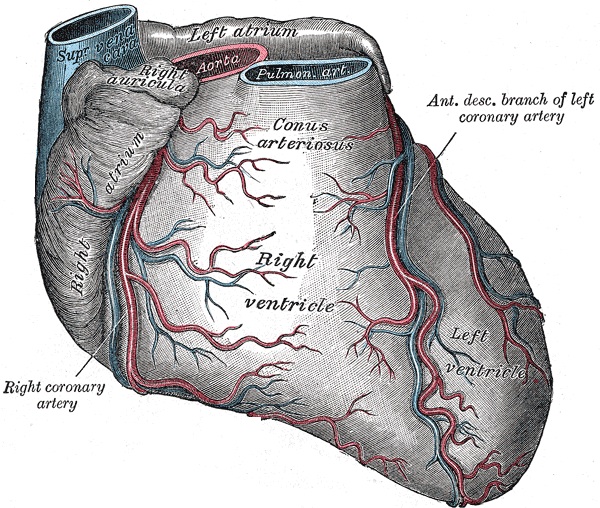 |
The smaller branches enter the myocardium and right angles and then divide into many more arteries and arterioles. The smaller structures support a very dense capillary network, with approximately one capillary for each cardiac fiber.42
Transmural (across the myocardial wall) blood flow distribution in accordance with moment to moment oxygen supply versus local demand change is supported by control of subendocardial and subepicardial vessel tone.42
Vasoactive substances released by coronary vascular endothelium provide circulatory regulation.
For example, a number of factors including pulsatile flow and hypoxia stimulate release of the coronary vasodilator prostacyclin.
|
|
|
Hypoxia and shear stress are two factors that increase production and release of nitric oxide (N-O) by increasing catalytic activity of nitric oxide synthase (NOS). By this mechanism, coronary vasodilatation occur secondary to N-O-dependent cGMP (cyclic GMP) mechanisms.42
Endothelium also elaborates vasoconstrictors such as the endothelins, thromboxane A2, and angiotensin in response to several exogenous and endogenous factors.42
|
|
|
Pathophysiological changes associated with coronary vascular disease can induce abnormalities between these vasodilator and vasoconstrictor effects. For example, a reduction in N-O release with a concurrent increase in endothelin synthesis.
Endothelins in addition to being vasoconstrictive also promote platelet adhesion which may increase thrombosis risk and cause smooth muscle proliferation.42
|
| This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |