|
|
|
Medical Pharmacology Chapter 33-34: Anticancer Drugs
Miscellaneous Anticancer Drugs:
Bleomycin (Blenoxane)
|
|
References
|
|
|
|
|
|
|
|
The bleomycins consists of a group of peptide polyketides.
Polyketides are described as "natural compounds containing alternating carbonyl and methylene groups (β-polyketones), by genetically derived from repeated condensation of acetyl coenzyme A (via malonyl coenzyme A), and usually the compounds derived from them by further condensations. Considered by many to be synonymous with the less frequently used terms acetogenins and ketides".13
Examples of polyketides include:
Geldanamycin (antibiotic)14
|
|
Doxycycline (antibiotic)14
|
|
Erythromycin (antibiotic)14
|
|
Aflatoxin B1 (carcinogen)14
|
|
Fungal mycotoxins are often polyketides.14
Bleomycin exhibits both antineoplastic and antimicrobial properties.16
Bleomycin binds to guanine bases in DNA, a process associated with oxidation of Fe2+ to Fe 3+ (ferous iron to ferric iron).
Associated with this reaction is production of superoxides and hydroxyl radicals which induce single-and double-stranded DNA breaks and deletions.
![]() The major
bleomycin toxicity is pneumonitis (sub acute or chronic) which may progress
to interstitial pneumonitis.16
The major
bleomycin toxicity is pneumonitis (sub acute or chronic) which may progress
to interstitial pneumonitis.16
As a group, the bleomycins are small glycopeptides.
![]() A mixture of
peptides (i.e. bleomycin) exhibits clinical activity against a number of
cancers including:
A mixture of
peptides (i.e. bleomycin) exhibits clinical activity against a number of
cancers including:
Hodgkin's disease
Testicular cancer
Cervical cancer
Penile cancer
Malignant pleural effusions.
Bleomycin when combined with vinblastine, etoposide and cisplatin is typically curative for testicular germ cell tumors.
![]() By contrast to
many antineoplastic drugs, bleomycin has nearly no hematopoietic toxicity,
although the agent is associated with pulmonary fibrosis.
By contrast to
many antineoplastic drugs, bleomycin has nearly no hematopoietic toxicity,
although the agent is associated with pulmonary fibrosis.
Bleomycin when incubated in vitro in cultured cell systems induces both single-and double-strand DNA breaks.11
Bleomycin is a cell-cycle specific drug exerting its principal effects in the G2 and M phases.10
Following incubation with bleomycin, the consequences of DNA breaks include chromosomal gaps, fragments, and deletions.
Bleomycin also targets both RNA and lipids. RNA and lipids are affected by bleomycin and derivative oxygen radicals.
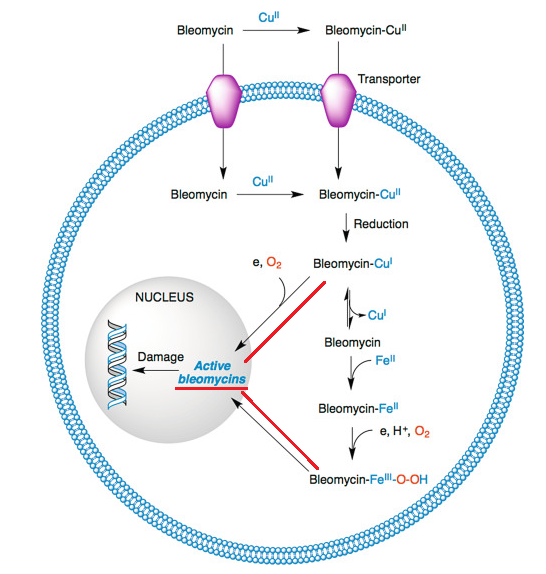
The multistep processes involved in the generation of Fe (II)-bleomycin-O2 complexes that directly promote DNA breaks.
The iron-binding domain and the DNA binding region are localized at opposite ends of the bleomycin peptide.3
|
|
|
Note that by contrast to typical DNA-damaging drugs, bleomycin does not modify nucleic acid bases nor affect phosphate linkages.11
Following administration of bleomycin, the parent drug forms a complex with copper, as Cu (II).11
Transport of the copper-bleomycin complex then occurs across cellular membranes with the transport being dependent on both the disaccharide component of bleomycin and the bound copper as Cu (II).
Following translocation into the cell, the Cu( II) complex is reduced to Cu (I) form and the Cu (I) complex is replaced by Fe (II) which is present at higher concentrations.
The Fe (II)-bleomycin complex is translocated into the nucleus where DNA damage that occurs.11
 |
|
Absorption, Distribution, Biotransformation, Excretion:
Using IV serum concentration as a reference, bleomycin is 100% absorbed with the intramuscular route of administration.9
By comparison, subcutaneous administration results in about 70% absorption with intrapleural administration associated with 45% absorption.
Volume of distribution (Vd) following IV administration is about 17.5 L/m2.
Bleomycin protein binding is estimated at about 1%.
The terminal half-life for administration (IV) is about two hours.
Following IV administration about 65% of the agent is excreted unchanged by the kidney; 40% for intrapleural administration.9
![]() Patients
exhibiting reduced renal function may experience elevated bleomycin blood
levels with attendant increased toxicity.18
Patients
exhibiting reduced renal function may experience elevated bleomycin blood
levels with attendant increased toxicity.18
Increased bleomycin toxicity may also be observed following cisplatin administration since cisplatin reduces bleomycin renal clearance.
Bleomycin is inactivated by the enzyme bleomycin hydrolase a.k.a. bleomycin hydrase (cytosolic cysteine proteinase).
Bleomycin hydrolase, a cytosolic aminopeptidase, catalyzes cleavage of the terminal amide, forming an inactive carboxylate metabolite.22
The amide is electron withdrawing; whereas, the carboxylate metabolite is an electron-donating species.
|
|
|
This change due to metabolism increases the ratio of ionized to un-ionized forms over 100-fold, virtually eliminating DNA affinity and terminating therapeutic efficacy.22
![]() Tumor
resistance to bleomycin could be caused by high concentrations of
bleomycin hydrolase.
Tumor
resistance to bleomycin could be caused by high concentrations of
bleomycin hydrolase.
By contrast, some tumors including squamous cell carcinoma have limited concentrations of bleomycin hydrolase which predicts good response to bleomycin.22
![]() This enzyme is
widely distributed in most issues with the exception of lung and
skin.18
This enzyme is
widely distributed in most issues with the exception of lung and
skin.18
|
|
|
Bleomycin may be administered for treatment of various cancers, including:1
Lymphoma
Malignant pleural effusions
Germ cell testicular and ovarian tumors
Bleomycin exhibits significant efficacy against testicular and ovarian germ cell tumors.
Furthermore, when bleomycin is combined with vinblastine and cisplatin or combined with etoposide and cisplatin, the combination protocol has been found often to be curative.
Hodgkin's disease
In Hodgkin's lymphoma bleomycin is a component of the:
ABVD protocol consisting of doxorubicin, bleomycin, vinblastine, dacarbazine as well as a part of the
BEACOPP regimen consisting of bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone.10
Squamous cell head and neck cancers20,21
![]() The major
advantage of bleomycin compared to other anticancer chemotherapeutic drugs
is limited myelosuppression.1
The major
advantage of bleomycin compared to other anticancer chemotherapeutic drugs
is limited myelosuppression.1
As result of reduced myelosuppression, bleomycin confers advantages when employed in combination protocols.
Many cutaneous toxicities have been reported including:
Hyperpigmentation
Hyperkeratosis
Erythema
Ulceration
Raynaud syndrome (unusual side effect).
Application of topical steroids are useful in managing "flagellate dermatitis" which manifests as an itching erythema on arms, scalp, back and hands.1
![]() The most
concerning adverse reaction to bleomycin is pulmonary toxicity which may
begin with a simple cough that can evolve to life-threatening pulmonary
fibrosis.
The most
concerning adverse reaction to bleomycin is pulmonary toxicity which may
begin with a simple cough that can evolve to life-threatening pulmonary
fibrosis.
Pulmonary complications describing clinical pulmonary toxicity is not an uncommon, given that about 5%-10% of patients are so afflicted.
Furthermore, about 1% of these patients die.
10% of patients exhibiting these pulmonary complications are those patients which have been treated with the higher cumulative dosing.
![]() In children
having received bleomycin, subclinical presentations a pulmonary toxicity
may occur in up to 50% of individuals as assessed by spirometry.11
In children
having received bleomycin, subclinical presentations a pulmonary toxicity
may occur in up to 50% of individuals as assessed by spirometry.11
Patients older than 70 are more likely to experience over toxicity especially if:
these individuals had prior chest radiotherapy or
if underlying renal dysfunction or emphysema was present or
if single doses >25 U/m2 were administered.11
|
|
|
|
|
|
|
|