Medical Pharmacology Chapter 35 Antibacterial Drugs
 |
 |
 |
 |
 |
 |
 |
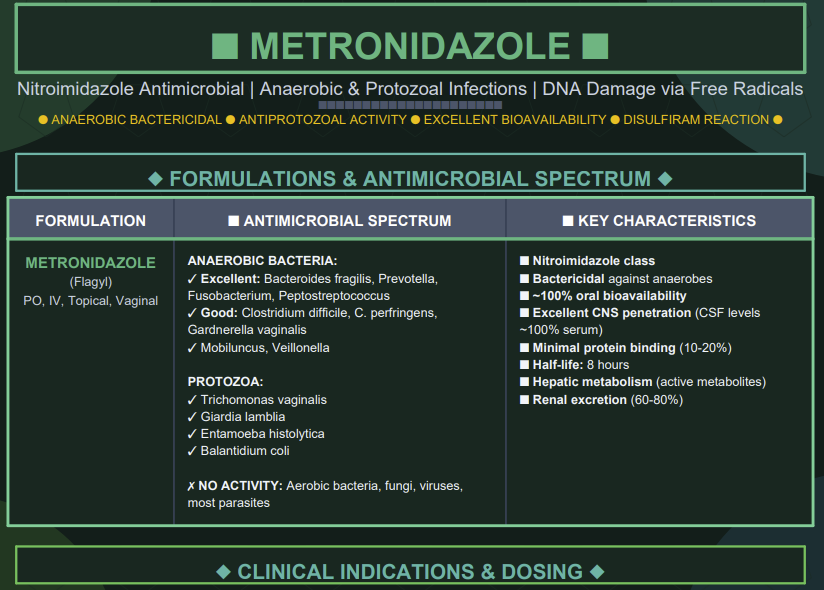
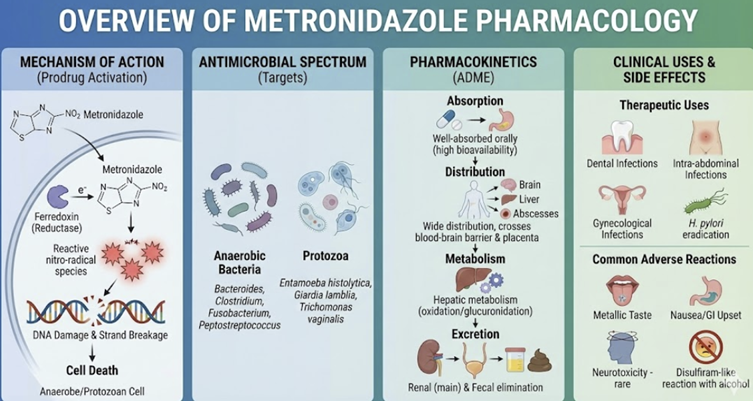
Metronidazole is a widely used nitroimidazole antibiotic and antiprotozoal agent with broad activity against anaerobic bacteria and certain protozoa/
Metronidizole is an important medication for treating anaerobic bacterial infections, protozoal infections and microaerophilic bacterial infections.1
This agent is cytotoxic to anaerobic microorganisms which can grow either in the presence or absence of oxygen (facultative anaerobic microorganisms).1
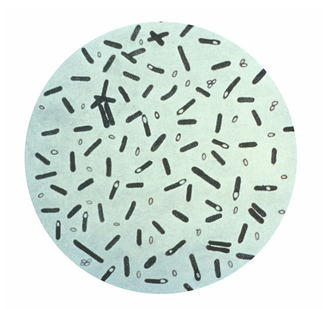
Specifically, metronidizole exhibits excellent activity against anaerobic bacteria such as Bacterioides, Closteridium, Fusobacterium, Peptococcus, Peptostreptococcus, and Eubacterium.2
 |
|
 |
|
 |
|
 |
|
Metronidizole shows lesser activity against Gardnerella and Helicobacter.2
 |
|
 |
|
Resistance to metronidizole is expected in Gram-positive anaerobes Actinomyces, Propionibacterium and Lactobacillus.2
In clinical practice (including primary care), metronidazole is valued for its bactericidal action, excellent tissue penetration, and oral availability.
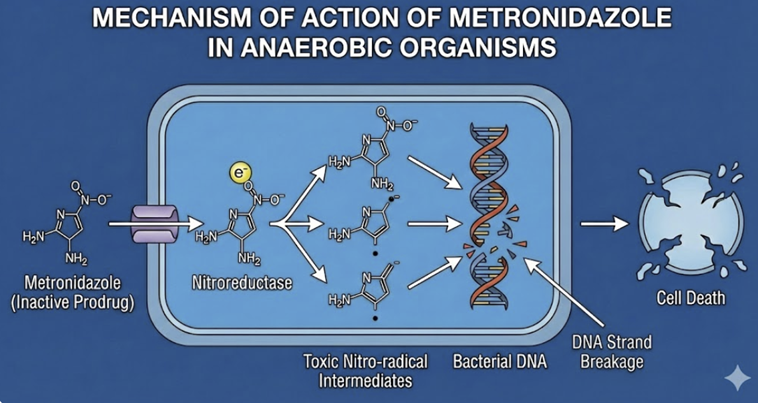 |
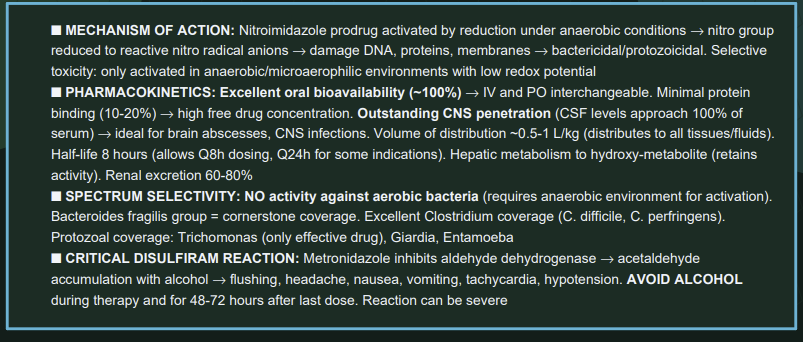
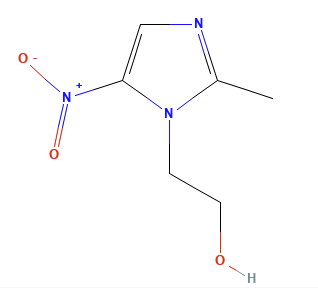
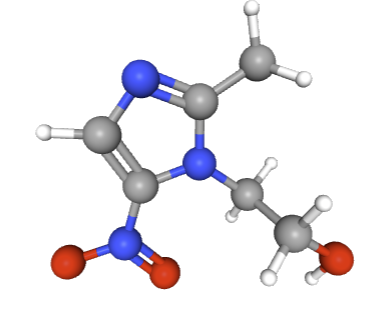
Metronidazole is a prodrug that becomes activated under anaerobic conditions to damage microbial DNA.2
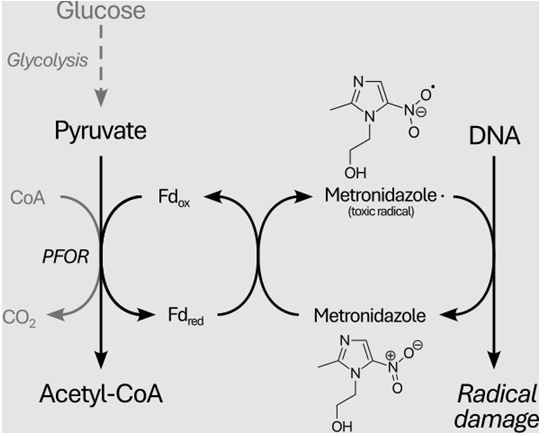
After passive diffusion into susceptible organisms, its nitro group is reduced by anaerobic cellular enzymes (such as ferredoxin-linked pyruvate oxidoreductase) to form a highly reactive nitroso radical anion.3
The radical anion targets DNA and other macromolecules, causing strand breakage and loss of helical structure, ultimately inhibiting nucleic acid synthesis and resulting in cell death.1 Other suggested mechanism of action for metronidazole involves an indirect inhibition of DNA synthesis and repair.5
Reductive activation in this setting occurs only in low-oxygen environments because oxygen competes for the electrons; hence metronidazole is selectively active against anaerobic and microaerophilic organisms and has minimal effect on aerobic human cells.3
Here oxygen effectively outcompetes
metronidazole for available electrons,
thereby preventing the drug's activation.
![]()
Anaerobes and certain protozoa “activate” metronidazole into a DNA-damaging agent, whereas human cells and aerobic bacteria do not.
This mechanism yields rapid, concentration-dependent bactericidal activity against susceptible microbes.1
 |
|
Antimicrobial Spectrum and Activity
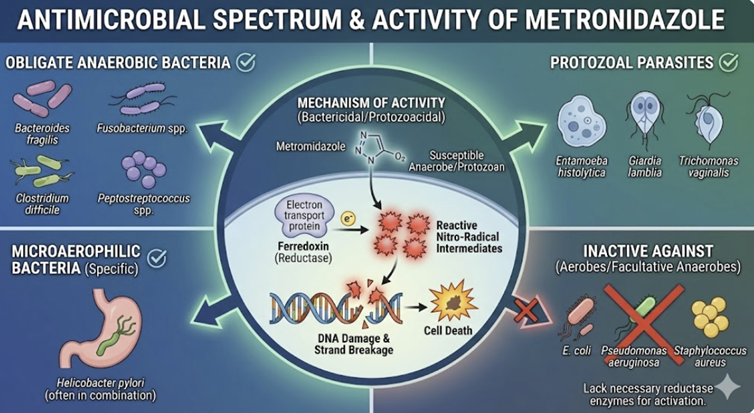 |
Metronidazole’s antimicrobial spectrum is limited to obligate anaerobes and select microaerophiles.
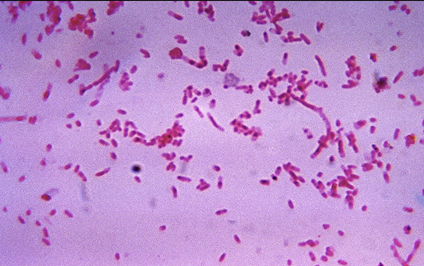
It is potently active against Gram-negative anaerobes (e.g. Bacteroides fragilis, Fusobacterium, Prevotella, Porphyromonas, Bilophila wadsworthia) and Gram-positive anaerobes (e.g. Clostridium species including C. perfringens and C. difficile, Peptostreptococcus).1
It also covers Gardnerella vaginalis (associated with bacterial vaginosis) and microaerophilic bacteria such as Helicobacter pylori.1
Metronidazole is bactericidal to susceptible anaerobes.
Metronidizole administration kills B. fragilis and C. perfringens more rapidly than clindamycin at equivalent doses.1
Metronidizole also exhibits excellent activity in anaerobic environments like abscess cavities.1,3
![]() Metronidizole has no
activity against aerobic bacteria (e.g.
Enterobacteriaceae, Pseudomonas, streptococci, staphylococci)
because these organisms cannot reduce the drug to its active
form, noting that in aerobic bacteria higher oxygen levels not
only reduce generation of activated metronidazole but also
increase recycling back to the unactivated metronidazole.3
Metronidizole has no
activity against aerobic bacteria (e.g.
Enterobacteriaceae, Pseudomonas, streptococci, staphylococci)
because these organisms cannot reduce the drug to its active
form, noting that in aerobic bacteria higher oxygen levels not
only reduce generation of activated metronidazole but also
increase recycling back to the unactivated metronidazole.3
![]() Metronidazole’s
role in bacterial infections is therefore
targeted to anaerobic
infections such as:
Metronidazole’s
role in bacterial infections is therefore
targeted to anaerobic
infections such as:
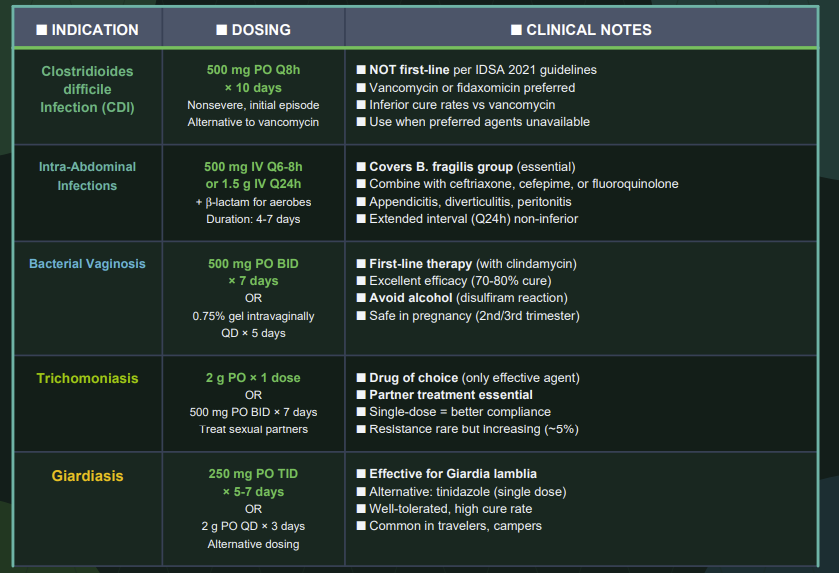
Intra-abdominal infections6
Complicated intra-abdominal infections are common and involve any mixture of anaerobic and aerobic bacteria.
Reasonable approaches may involve single-agent treatment with carbapenem as well as combination treatment with metronidazole and cephalosporin or fluorquinolone.
Despite long-term clinical use, generally resistance to metronidazole remains low (2015).6,7
Aspiration pneumonia and lung abscess (anaerobic oral flora)8
In the case of lung abscess, the infection tends to be polymicrobial and if metronidazole is used pairing it with another agent (e.g. penicillin) would be likely required to obtain the necessary coverage in this setting.9
Deep soft tissue infections (e.g. diabetic foot with anaerobes)10
A number of antimicrobials that prove effective may be used in treating this condition.10
Brain abscess (often polymicrobial with anaerobes)11
The use of cefotaxime, a third-generation cephalosporin, extends coverage compared to metronidazole alone to include Gram-positive, Gram-negative as well as anaerobic bacteria.12
Dental/orofacial infections (anaerobic oral organisms).13
It is also used for surgical prophylaxis in colorectal surgery to prevent anaerobic infections, often in combination regimens.1
Metronidizole continues to be effective in treating Trichomonas vaginalis and the nitroimidazoles represents the only class of medications with demonstrated efficacy against T. vaginalis infections.14
Metronidazole is effective in treating giardiasis, although antimicrobial resistance has been reported. Metronidazole is drug most commonly used in the United States for treating giardiasis.
Another agent, tinidazole, also approved in the United States is the first-line drug outside the United States.15
Mechanistically, resistant protozoal strains often have decreased pyruvate-ferredoxin oxidoreductase activity or lower ferredoxin levels, which impairs metronidazole activation.3
Entamoeba histolytica has not shown significant resistance clinically.3
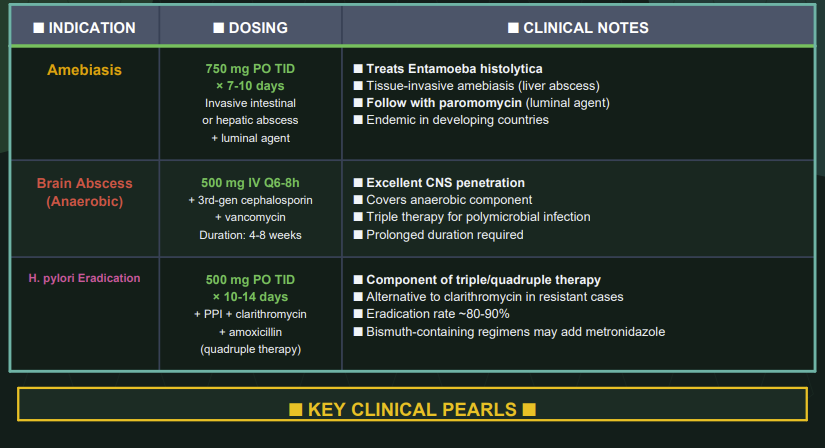
Bacterial and Parasitic Resistance
Anaerobic Bacteria
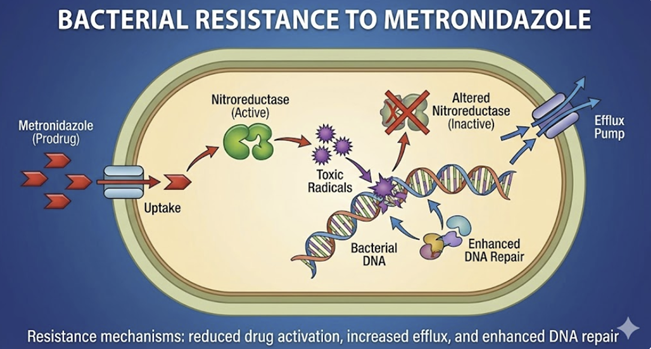 |
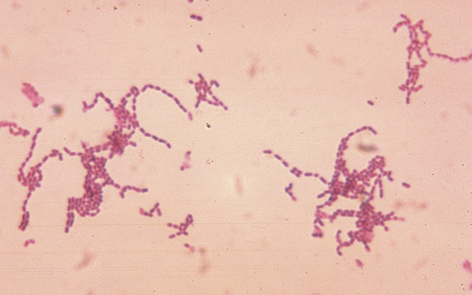
Some Bacteroides and other anaerobes have acquired nim genes (nimA–nimK) encoding 5-nitroimidazole reductases that convert metronidazole to non-toxic amine derivatives before it can damage DNA.3
Strains harboring nim genes show decreased susceptibility or clinical resistance to nitroimidazoles.16
Other resistance mechanisms in bacteria include increased expression of drug efflux pumps, altered redox environment (elevated oxygen or altered electron transport that impairs drug activation), and biofilm formation reducing drug penetration.3
![]() Clostridioides
difficile has shown increasing treatment failure rates
with metronidazole.
Clostridioides
difficile has shown increasing treatment failure rates
with metronidazole.
Reduced susceptibility of C. difficile isolates has been reported, corresponding to higher recurrence rates.17
Because of this finding, recent guidelines have de-emphasized metronidazole monotherapy in C. difficile infection.
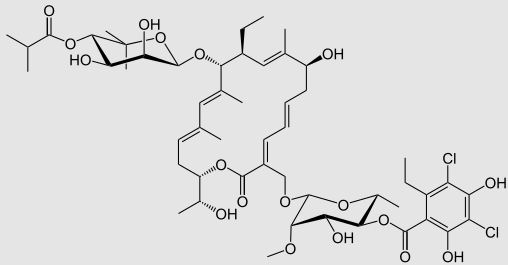
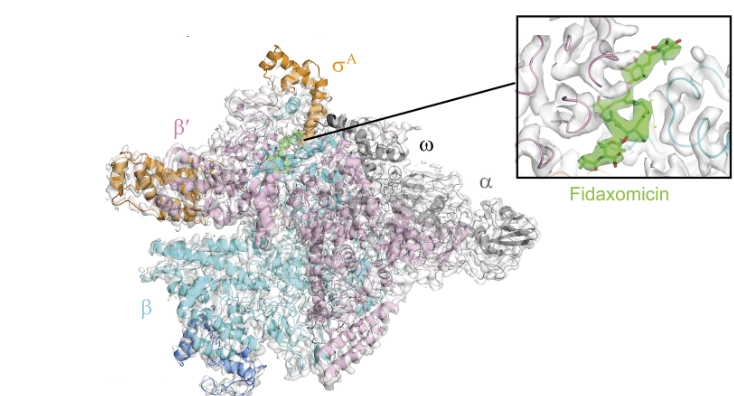
Metronidizole is no longer viewed as the first-line antibiotic choice for Clostridium difficile infection (vancomycin or fidaxomicin are now recommended over metronidazole for initial Clostridium difficile presentations.)1,18
This assessment is based on the 2017 Update by the Infectious Diseases Society of (AmericaIDSA) and Society for Healthcare Epidemiology of America (SHEA)18
The status of metronidizole in terms of treating Clostridium difficile was further considered in the 2021 update to the IDSA/SHEA Clostridioides difficile guidelines.19
![]() Not only is
metronidizole describe is no longer a first-line antibiotic
choice (1), the guidelines now prioritize the use of
fidaxomicin over vancomycin for treating initial and recurrent
Clostridioides difficile infection (CDI).20
Not only is
metronidizole describe is no longer a first-line antibiotic
choice (1), the guidelines now prioritize the use of
fidaxomicin over vancomycin for treating initial and recurrent
Clostridioides difficile infection (CDI).20
 |
|
 |
|
Fidaxomicin (Fdx) inhibits RNA polymerase (RNAP), thus targeting Clostridium difficile (Cdiff) with limited effects on gut commensals which decreases the likelihood of Cdiff recurrence.21
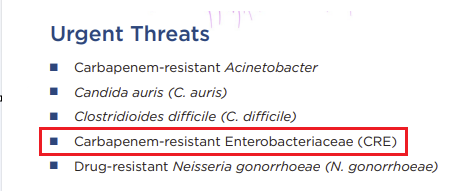
Clostridioides difficile (Cdiff) Isaac Gram-positive, toxin-producin intestinal bacterium which upon infecting the human gut induces lethal diarrhea (Cdiff infections or CDIs).21
"With the alarming increase in affection with the alarming increase in infections caused by highly pathogenic variance, Cdiff has been designated an 'urgent threat' by the CDC.
"Broad-spectrum antibiotics like vancomycin and Metronidazolea used to treat CDIs, but these antibiotics decimate the normal gut microbiome, paradoxically priming the gastrointestinal tract become more prone to CDI recurrences."21 for the quotation, 23,24
 |
|
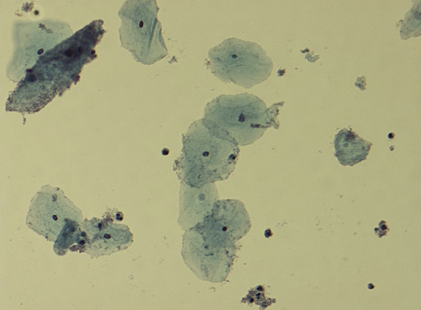
![]() H. pylori is
another organism with notable metronidazole resistance with
resistance rates exceeding 50-80% in some regions.19
H. pylori is
another organism with notable metronidazole resistance with
resistance rates exceeding 50-80% in some regions.19
In a recent cross-sectional study involving the Egyptian population, about 44% of isolates proved resistant to metronidizole with 12%, 4.5% and 55.4% exhibiting resistance to clarithromycin, amoxicillin and levofloxacin.25
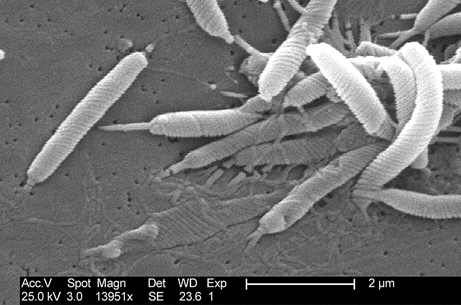
Helicobacter pylori is a microaerophilic (requiring reduced oxygen levels compared to atmospheric levels) Gram-negative bacterium associated with the human gastric mucosa (about 44% in adults in about 35% in children and adolescents). Warren and Marshall27 identified H. pylori association with chronic gastritis and peptic ulcer disease28 which dramatically changed clinical management.26
Protozoa
Resistance in Trichomonas vaginalis and Giardia lamblia has been observed in some cases of treatment failure.14,29
Mechanistically, resistant protozoal strains often have decreased pyruvate-ferredoxin oxidoreductase activity or lower ferredoxin levels, which impairs metronidazole activation.30
Some T. vaginalis isolates also develop higher oxygen tolerance (reducing activation of the drug).3
These parasites may still respond to higher doses or longer courses of metronidazole, or to alternative nitroimidazoles (like tinidazole).31,32
A number of alternative drugs and drug combinations to the nitroimidazoles in the case of resistance.
Some observational studies and some clinical studies describe available options.33
Metronidazole resistant Entamoeba histolytica has been described as a developing concern, although metronidizole remains the most commonly used agents against amoebiasis.34
August, 2025
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |